
When it comes to nursing practice, every decision counts—especially in moments when patient safety and care are on the line. Nursing exemplars are essential for showcasing the critical thinking and judgment that every nurse brings to their role.
In this article, we’ll explore the importance of nursing exemplar examples and how they provide insight into your clinical skills, decision-making, and personal growth. You’ll find guidance on writing a compelling exemplar, tips for highlighting measurable outcomes, and common mistakes to avoid. We’ll also discuss how to align your exemplars with Magnet® recognition standards and other professional goals.
What Is a Nursing Exemplar?
A nursing exemplar is a reflective story describing a clinical situation where your actions and decisions made a positive impact on patient care. It highlights your clinical reasoning, decision-making, and ability to respond effectively in real-life scenarios.
Nursing exemplars are often included in portfolios or Magnet® applications. They focus on the nurse’s perspective—what you observed, how you responded, and the lessons learned.
Unlike case studies or chart notes, a nursing exemplar is personal. It showcases your thinking process, not just actions. It allows you to reflect on your growth as a nurse and demonstrate your competence.
Why Nursing Exemplar Examples are Important
A Tool for Reflection and Professional Growth
Writing nursing exemplars offers a chance to evaluate your actions and the outcomes that followed. This process encourages continuous learning and improvement in your practice.
By reflecting on real situations, you gain a better understanding of your decision-making. This allows you to approach similar challenges more effectively in the future.
Showcasing Clinical Judgment
Nursing exemplars demonstrate your ability to assess a situation, make informed decisions, and act accordingly. They provide clear evidence of your clinical reasoning and problem-solving skills.
These exemplars not only show what you did, but why you made certain decisions. This is key for performance reviews and career development.
Read more on clinical judgment and examples
Relevance for Magnet® Recognition
In Magnet®-designated hospitals, nursing exemplars play a crucial role. They show how nursing care directly impacts patient outcomes, such as improving safety or patient satisfaction.
Including measurable outcomes in your exemplar strengthens your case for Magnet® recognition. These results provide tangible evidence of your contributions to the hospital’s goals.
Nursing Exemplar Template (Copy, Paste, and Fill)
To make writing your nursing exemplar easier, here’s a simple template you can follow. This structure will help you organize your thoughts and ensure you include all the necessary components.
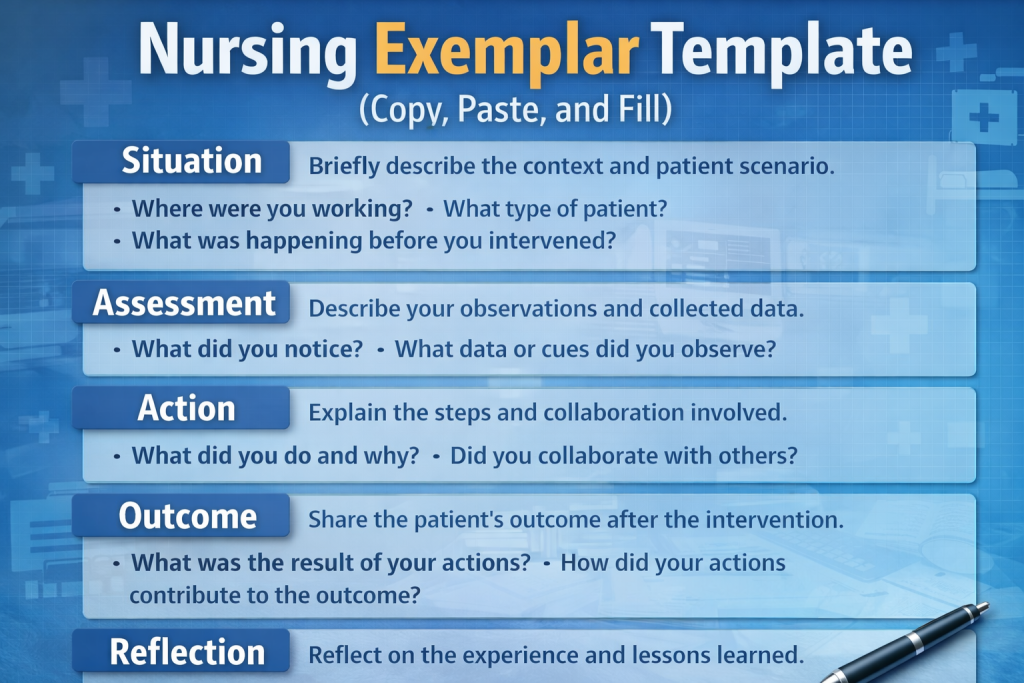
Situation/Context
- What was happening?
Describe the setting, type of patient, and what led up to the situation. - Why is it important?
Providing context helps the reader understand the environment and conditions that influenced your decisions.
Assessment
- What did you notice?
Explain your observations. These could be clinical signs, patient feedback, or changes in condition. - What data or cues did you use?
Refer to vital signs, lab results, or patient behavior that guided your assessment.
Action
- What did you do and why?
Describe the steps you took in response to the situation. - Did you collaborate with others?
Mention if you involved other team members, like doctors or specialists, and explain how their input influenced your approach.
Outcome
- What was the result of your actions?
Highlight measurable improvements, such as stabilization of a patient’s condition or improvement in patient satisfaction. - Was the outcome positive or negative?
Be honest about the results, focusing on what worked well and what could have been done differently.
Reflection
- What did you learn from this experience?
Reflect on how the situation shaped your practice and what you’d do differently next time. - How has it influenced your clinical reasoning?
Consider how this experience changed or reinforced your approach to patient care.
Example 1: Nursing Exemplar Example— Patient Safety and Escalation
Situation
I was working on the post-operative surgical unit when I noticed a patient who had recently undergone a hip replacement surgery. Initially, the patient was stable with no major complications. However, about two hours after receiving pain medication, the patient’s breathing became noticeably shallow, and their oxygen saturation levels began to drop.
Assessment
Upon noticing the patient’s respiratory distress, I immediately rechecked the vital signs. The oxygen saturation level had decreased from 94% to 86%, and the patient was becoming increasingly lethargic. These signs were concerning, and I suspected early signs of respiratory depression due to the recent pain medication.
Action
I immediately stopped the pain medication infusion to prevent further respiratory depression. To assist the patient’s breathing, I elevated the head of the bed and increased the oxygen flow. I contacted respiratory therapy for an evaluation and informed the physician of the situation. While waiting for respiratory therapy, I closely monitored the patient’s vital signs and stayed with the patient to provide reassurance.
Outcome
Within 10 minutes of the intervention, the patient’s oxygen saturation improved to 92%, and their breathing became more regular. The patient was able to avoid an ICU transfer. The physician acknowledged the quick response and appreciated the early intervention, which helped stabilize the patient’s condition before it escalated.
Reflection
This experience reinforced the importance of early recognition of respiratory distress and early intervention in preventing complications. By acting quickly, I was able to avoid a potentially dangerous situation. Since then, I have made it a point to monitor post-operative patients more closely for any signs of respiratory issues, especially after administering pain medications. This experience has shaped my approach to post-op care, ensuring I remain vigilant and proactive in managing potential complications.
Example 2: Nursing Exemplar Example — Compassion and Communication
Situation
I was working on the oncology unit when a middle-aged patient, recently diagnosed with cancer, was informed by the doctor about their condition. Upon hearing the diagnosis, the patient became visibly upset, breaking down in tears. They were struggling to process the information, expressing fear and uncertainty about what this diagnosis meant for their future.
Assessment
I noticed the patient’s emotional distress. They were crying, shaking, and appeared overwhelmed. While their vital signs were stable, their emotional state was clearly affecting their ability to absorb the information. It was clear that this was a moment when the patient needed emotional support, rather than immediate medical intervention.
Action
Recognizing the importance of addressing the patient’s emotional needs, I took a few extra minutes to sit with them and listen. I acknowledged their feelings and reassured them that it was okay to feel overwhelmed and scared. I didn’t rush them through the moment but instead created a safe space for them to express their emotions. I also arranged for a consultation with the hospital’s social worker, ensuring the patient had additional support to navigate the emotional challenges ahead.
Outcome
The patient was grateful for the time I took to listen and for the reassurance I provided. Their emotional state calmed, and they were able to process the diagnosis more effectively. Later, the social worker met with the patient and offered further counseling and support. The patient later expressed relief in knowing they weren’t alone in dealing with their emotions and that support was available.
Reflection
This experience reinforced for me that compassionate communication is just as important as clinical care. Sometimes, being present for a patient and allowing them space to express their feelings can make a significant difference in their ability to cope with a difficult diagnosis. Since then, I’ve made it a point to check in on the emotional and psychological needs of my patients, especially in challenging moments. I’ve learned that offering empathy and a listening ear is crucial to holistic patient care.
Example 3: Nursing Exemplar Example — Clinical Judgment and Prioritization
Situation
During a particularly busy shift on the medical-surgical unit, I was caring for a diabetic patient who had stable glucose levels earlier in the day. However, later in the shift, I noticed that the patient’s blood glucose levels began to drop unexpectedly, despite them having been well-managed previously.
Assessment
Upon checking the patient’s glucose levels, I found that the reading was 65 mg/dL—below the expected range for the patient’s condition. This drop was concerning, especially since the patient had no other signs of distress and their vital signs had remained stable throughout the day.
Action
I first recalibrated the glucose meter to ensure the reading was accurate, then verified the result with a lab test. The lab confirmed the low glucose level, and upon reviewing the patient’s chart, I discovered an insulin dosing error earlier in the day. I immediately corrected the error and administered a small dose of glucose to bring the levels back to normal. I monitored the patient closely over the next few hours, adjusting their care as needed. I also notified the attending physician and collaborated with the pharmacy to review the insulin dosing process for future reference.
Outcome
The patient’s glucose levels stabilized after the intervention and returned to a safe range. They avoided hypoglycemia and any associated complications. The physician was updated on the situation and appreciated the quick action taken to correct the error and prevent further issues. Additionally, the pharmacy implemented a new verification step to ensure the correct insulin dosage is administered going forward.
Reflection
This experience highlighted the importance of double-checking critical data and verifying readings, especially when they don’t align with expectations. I learned that in high-pressure situations, it’s easy to overlook small discrepancies, but it’s essential to address them promptly to avoid complications. Since then, I have adopted a more thorough approach when reviewing patient data and insulin dosages, always verifying measurements and working collaboratively with the team when discrepancies arise. This experience has strengthened my clinical judgment and prioritization skills, ensuring that I’m prepared to act swiftly when needed.
Writing a Strong Nursing Exemplar Example: Tips, Tricks & Common Mistakes
Writing a strong nursing exemplar involves more than just telling a story—it’s about effectively demonstrating your clinical judgment and professional growth. Here are some key tips for writing a clear and impactful exemplar, followed by common mistakes to avoid.
Tips for Writing a Strong Nursing Exemplar
- Stay Focused
Focus on one clear event or situation. Avoid trying to cover an entire shift or multiple scenarios. The more specific you are, the clearer your example will be. - Be Specific About Actions
Describe the exact steps you took, not just the general outcome. This helps demonstrate your critical thinking and decision-making skills. - Use Active Voice
Write in the first person and use active voice. Phrases like “I assessed” or “I called the physician” are stronger and more personal than passive voice. - Include Measurable Outcomes
Whenever possible, include measurable results. For example, if a patient’s condition improved, provide specific data or observations that support the change, such as stabilized vital signs or improved patient satisfaction scores. - Reflect on the Experience
Conclude with reflection. Explain what you learned from the situation and how it has influenced your practice. This is crucial for showing personal and professional growth.
Common Mistakes to Avoid
- Being Too Vague
Avoid using general phrases like “I helped the patient.” Instead, specify what actions you took, such as “I administered oxygen and elevated the head of the bed to improve breathing.” - Writing Like a Chart Note
Nursing exemplars are not chart notes. They should be written in full sentences with natural language. Avoid shorthand and abbreviations. For example, instead of “Pt. c/o pain,” write “The patient reported severe pain.” - Forgetting Reflection
A nursing exemplar without reflection is incomplete. Always include a section where you explain what the situation taught you and how it has changed your approach to care. - Overwriting or Adding Drama
Stick to the facts and avoid exaggerating the emotions of the situation. A good exemplar is authentic and focused on the patient’s care, not on dramatic storytelling. - Skipping the Outcome
Every exemplar should include the outcome of your actions. Readers need to know whether your interventions were successful, and including measurable results strengthens the impact of your exemplar.
Final Takeaways
Nursing exemplars are essential tools for showcasing your clinical judgment, decision-making, and professional growth. They allow you to reflect on real-world situations where your actions led to positive patient outcomes. By writing strong, reflective nursing exemplars, you demonstrate your ability to think critically and provide evidence-based care.
Key Points to Remember:
- Be Specific: Focus on one event and provide clear details about your actions and their outcomes.
- Include Reflection: Always reflect on what you learned from the experience and how it influenced your practice.
- Use Measurable Outcomes: Whenever possible, include data or measurable results to show the impact of your actions.
- Keep it Concise: Aim for a focused, clear narrative without unnecessary details. Stick to the situation, assessment, action, outcome, and reflection.
By following these principles, you can create nursing exemplars that are both meaningful and effective. Whether you’re documenting your progress for career advancement or working toward Magnet® recognition, exemplars provide valuable evidence of your nursing skills and growth.
FAQs
How Long Should a Nursing Exemplar Be?
Most nursing exemplars should be between 300–600 words. The key is to keep your story focused and concise. Avoid unnecessary details and stick to the main points: the situation, what you did, the outcome, and your reflection.
Can Nursing Exemplars Be Used for Magnet® Documentation?
Yes, nursing exemplars are essential for Magnet® documentation. They help demonstrate how nursing care directly contributes to patient outcomes. For Magnet® recognition, your exemplar should include measurable results, such as improved patient safety, reduced infection rates, or enhanced patient satisfaction.
What’s the Difference Between an Exemplar and a Case Study?
A case study focuses on the patient’s medical condition, treatments, and outcomes. It provides detailed clinical information.
A nursing exemplar, on the other hand, focuses on your actions as a nurse—how you assessed, made decisions, and contributed to the care process. It’s more about your clinical judgment and professional growth.
How Can I Make My Exemplar Stand Out?
To make your nursing exemplar stand out:
- Be specific: Focus on one clear situation and describe your actions in detail.
- Include measurable outcomes: Show the impact of your actions, such as improved patient metrics.
- Reflect honestly: Talk about what you learned from the experience and how it shaped your practice.
Can Exemplars Be Used by Students or Only Practicing Nurses?
Both students and practicing nurses can write nursing exemplars.
- For students, exemplars help build reflective and critical thinking skills.
- For practicing nurses, exemplars document professional growth and can be used in performance evaluations, job applications, or Magnet® submissions.

