In home care nursing, your notes are more than just paperwork—they’re an essential part of patient care. As a home care nurse, your documentation provides a record of your patient’s journey and serves as a communication tool between you, other healthcare providers, and the patient’s family. But we know—it’s not always as simple as jotting down a few sentences.
Effective home care nursing notes help ensure that every patient gets the best care possible, no matter who is providing it. They’re essential for continuity, accuracy, and compliance, and they play a crucial role in ensuring that your professional actions are legally protected.
In this guide, we’ll explore everything you need to know about writing home care nursing notes. We’ll cover why these notes matter, what to include in them, and how to make sure they’re clear, complete, and compliant with legal and professional standards.
What Are Home Care Nursing Notes?
At its core, home care nursing notes are written records that document everything you observe, do, and plan for a patient while providing care in their home. Think of them as your “official record”—a snapshot of the care provided and the patient’s progress over time.
These notes serve multiple purposes: they guide your ongoing care, inform other healthcare providers about the patient’s status, and provide a detailed record that can be referred to in case of legal or insurance questions. They are vital for coordinating with other healthcare providers (doctors, physical therapists, etc.), ensuring consistent care across visits.
In short, home care nursing notes help everyone involved in the patient’s care understand exactly what’s going on, why certain actions are being taken, and what still needs to be done. Without these notes, there’s a risk of confusion, errors, and potentially missed opportunities to improve the patient’s care.
Why Are Home Care Nursing Notes Important?
- Communication Tool: You’re often working alone or with limited supervision, so clear notes ensure other healthcare professionals can follow along with your observations and interventions.
- Patient Safety: Accurate notes help identify trends—whether that’s improving health, complications, or responses to treatments. They are crucial for adjusting care as needed.
- Legal Protection: Home care nursing notes are often used as legal documents. If there’s ever a question about what happened during a visit, your notes are the first place someone will look to understand the care provided.
- Billing and Insurance: Proper documentation is often required for insurance claims. It helps justify the services provided and ensures that you are paid correctly for your work.
In a way, these notes are your professional “snapshot” of patient care—a comprehensive record of what you’ve observed, what actions you’ve taken, and what the next steps are in your patient’s care plan.
How to Write and Key Elements to Include in Every Note
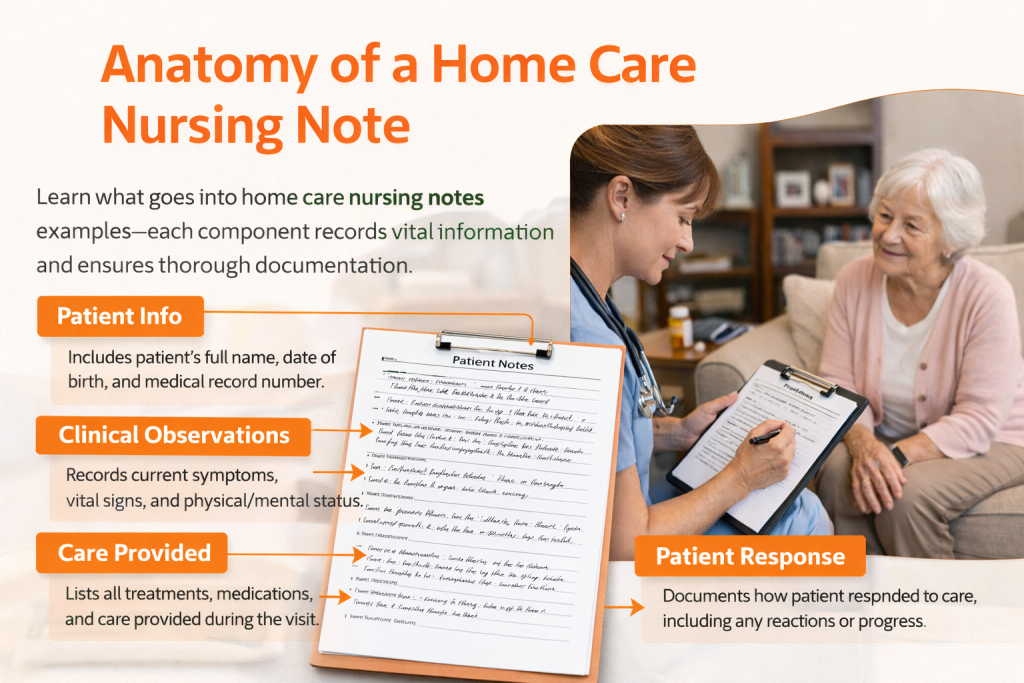
When you sit down to write home care nursing notes, it’s essential to include the right components. Each part of your note helps build a clear, accurate picture of the patient’s current condition and the care you’ve provided. By following a consistent structure, you can ensure your notes are professional, thorough, and useful for anyone reviewing them.
Here are the core components you should include in every home care nursing note:
| Section | What to Include | How It’s Used in Practice |
| Patient Information | Patient’s full name, date of birth, medical record number (if applicable), and other identifying details | Keeps documentation tied to the correct patient and allows other healthcare providers to quickly locate and verify records |
| Date and Time of Visit | Exact date and time of the home visit | Creates a clear timeline of care and supports documentation required for billing and insurance |
| Reason for Visit | Short explanation of why the visit occurred (e.g., post-surgical follow-up, medication management, chronic condition monitoring) | Provides context for the visit and sets expectations for what the note will cover |
| Clinical Observations | Objective findings such as physical condition, mental status, symptoms, and vital signs | Paints a clear picture of the patient’s current status and highlights changes over time |
| Interventions & Care Provided | All care delivered during the visit, including medications, wound care, exercises, education, or assistance with daily activities | Documents exactly what actions were taken during the skilled nursing visit |
| Patient Response | How the patient reacted to care (tolerated well, discomfort noted, improvement observed) | Shows how effective the interventions were and informs future care decisions |
| Plan for Follow-up | Next steps such as future visits, referrals, care plan changes, or instructions for patient or caregiver | Keeps care coordinated and ensures continuity between visits |
| Signature | Nurse’s name, credentials, and signature (plus team members if applicable) | Confirms accountability and identifies the professional responsible for the note |
Common Types of Home Care Nursing Notes
There are several types of home care nursing documentation examples used depending on the specific care being provided. Here are some of the most common types of nursing notes you may encounter in home care:
1. Initial Assessment Notes
These are the first notes you write when you begin caring for a patient. Initial assessment notes are crucial for establishing a baseline of the patient’s health. They should include a detailed history, any current medical conditions, medications, allergies, and the care plan going forward.
2. Progress Notes
These notes document the ongoing progress of the patient. Progress notes highlight any changes in the patient’s condition, response to interventions, and any adjustments made to the care plan. These are essential for tracking improvements or setbacks in the patient’s recovery.
3. SOAP Notes
The SOAP format is a widely used method for organizing nursing documentation:
- S (Subjective): The patient’s reported symptoms or concerns.
- O (Objective): Observable data, such as vital signs or physical findings.
- A (Assessment): The nurse’s clinical judgment about the patient’s condition.
- P (Plan): The actions to be taken, including follow-up care.
SOAP notes are an effective way to structure your documentation, making it easier for other healthcare providers to follow.
4. Narrative Notes
Narrative nursing notes in home care are a more detailed and free-form method of documenting patient care. These notes may include descriptions of patient interactions, the nurse’s observations, and any changes in the patient’s condition. They are often used for more complex situations where other formats might not capture the full picture.
5. Discharge Notes
When a patient is being discharged from home care, discharge notes are used to document the final status of the patient’s health and outline any ongoing care instructions. These notes may also include recommendations for further care, referrals to specialists, or home modifications.
6. Daily Visit Notes
Daily visit notes are used to document each home visit. These notes can be more concise than others but still should include key details such as the patient’s current condition, the care provided, and the plan for the next visit.
Home Care Nursing Notes Examples
In this section, we’ll provide several home care nursing notes examples that cover a variety of situations you may encounter in your nursing practice. Each example follows the structure we’ve outlined earlier—ensuring clarity, accuracy, and completeness in the documentation.
11. home health nursing notes example (SOAP)
Date & Time: January 18, 2026, 11:00 AM
Patient Information: Sarah Mitchell, DOB 08/23/1956, MRN 445566
Reason for Visit: Chronic low back pain assessment
S (Subjective):
- Patient reports persistent lower back pain for the past 3 months.
- Describes pain as “aching” and rates it 6/10 on the pain scale.
- Pain worsens with bending and standing for prolonged periods.
- Reports difficulty sleeping due to discomfort.
O (Objective):
- Patient ambulates with a slight limp, no visible deformities in posture.
- Tenderness noted in the lumbar region.
- Vital signs: BP 125/80, pulse 78 bpm, temp 98.6°F.
- No swelling or redness in lower back.
A (Assessment):
- Chronic low back pain, likely musculoskeletal in nature.
- Possible muscle strain or disc degeneration due to patient’s reported symptoms and limited mobility.
- No signs of acute injury or systemic issues.
P (Plan):
- Continue conservative management with NSAIDs for pain relief.
- Recommend physical therapy for strengthening and mobility exercises.
- Follow-up in one week for reassessment of pain and mobility.
Signature: Nurse Claire Roberts, RN
12. Narrative home care nursing notes example
Date & Time: January 19, 2026, 1:00 PM
Patient Information: Michael Thompson, DOB 09/12/1970, MRN 789123
Reason for Visit: Routine health check-up and blood pressure monitoring
Clinical Notes:
Michael was observed to be in a generally good mood during the visit. He stated that he has been feeling “well” overall, though he occasionally experiences mild dizziness when standing up too quickly. Blood pressure was measured at 130/85 mmHg, which is higher than his baseline of 120/80, but still within an acceptable range. He reports being compliant with his medication regimen, and his recent blood tests came back normal, showing no signs of kidney damage or other complications.
We discussed the importance of continuing his blood pressure medication and maintaining a low-salt diet. Michael is aware of the lifestyle changes that need to be made to manage his condition better, including reducing stress and exercising more frequently. He expressed interest in starting a walking routine to improve his cardiovascular health.
At the end of the visit, Michael seemed motivated to stick to the plan we discussed, and we agreed to schedule a follow-up visit in one month to monitor his blood pressure and overall health.
Signature: Nurse Olivia Hall, RN
13. Discharge Note Example
Date & Time: January 20, 2026, 3:00 PM
Patient Information: Jessica Clark, DOB 02/05/1982, MRN 654321
Reason for Visit: Post-hospital discharge monitoring following pneumonia recovery
Clinical Observations:
- Patient was discharged from the hospital on January 18, 2026, following successful treatment of pneumonia.
- No signs of infection at this time, and patient reports feeling “much better.”
- Vital signs: BP 118/75, pulse 72 bpm, oxygen saturation 98% on room air.
- No respiratory distress or cough, though patient still has mild fatigue.
Interventions & Care Provided:
- Reinforced discharge instructions regarding antibiotic regimen, breathing exercises, and signs of relapse.
- Instructed patient to gradually increase physical activity as tolerated, emphasizing the importance of rest.
- Discussed follow-up with primary care provider in one week and chest X-ray in two weeks to monitor lung recovery.
Patient Response:
- Patient expresses understanding of post-discharge care instructions.
- No concerns raised regarding medications or future appointments.
Plan for Follow-up:
- Follow-up visit scheduled for January 25, 2026, to monitor recovery.
- Ensure adherence to prescribed medications and encourage continued physical rest.
Signature: Nurse Rachel Adams, RN
14. Progress home health nursing notes example
Date & Time: January 20, 2026, 9:45 AM
Patient Information: Edward Williams, DOB 12/05/1960, MRN 334455
Reason for Visit: Progress check for diabetes and hypertension management
Clinical Observations:
- Patient reports feeling more energetic after implementing dietary changes, but blood pressure remains higher than desired.
- Blood pressure reading: 145/90 mmHg.
- Blood sugar level: 130 mg/dL before lunch (recently improved).
- Patient states that he’s been exercising regularly but still feels stressed at work.
Interventions & Care Provided:
- Reviewed blood pressure medication and suggested adding a beta-blocker to help manage hypertension.
- Provided additional education on managing stress and encouraged relaxation techniques.
- Discussed continuing regular monitoring of blood sugar levels and maintaining a low-sodium diet.
Patient Response:
- Patient acknowledges stress levels and plans to seek stress management support through therapy.
- Expressed willingness to follow through with medication adjustments and lifestyle changes.
Plan for Follow-up:
- Follow-up visit scheduled for February 2, 2026, to assess blood pressure control and stress management progress.
Signature: Nurse Mark Johnson, RN
15. Daily Visit home care nursing notes example
Date & Time: January 21, 2026, 8:00 AM
Patient Information: Hannah Foster, DOB 03/19/1948, MRN 112233
Reason for Visit: Daily monitoring for heart failure
Clinical Observations:
- Patient appears in stable condition, but reports occasional shortness of breath with exertion.
- Weight: 160 lbs, unchanged from previous visit.
- Vital signs: BP 120/70, pulse 80 bpm, respiration rate 18 breaths per minute.
Interventions & Care Provided:
- Administered diuretic as per medication plan to prevent fluid retention.
- Educated patient on signs of fluid overload and instructed to monitor weight daily.
- Encouraged patient to rest and avoid strenuous activity to reduce heart strain.
Patient Response:
- Patient reports no new symptoms but mentioned mild fatigue.
- Verbalized understanding of fluid monitoring and diuretic usage.
Plan for Follow-up:
- Continue current care plan.
- Next daily visit scheduled for January 22, 2026, for routine monitoring.
Signature: Nurse Jessica Turner, RN
1. Post-Surgical Follow-Up home health nursing notes example
Date & Time: January 15, 2026, 9:00 AM
Patient Information: John Doe, DOB 01/23/1950, MRN 123456
Reason for Visit: Post-surgical follow-up for knee replacement
Clinical Observations:
- Patient appears alert and oriented to person, place, and time.
- Surgical site clean, no signs of infection, minimal swelling noted.
- Pain level reported as 4/10, treated with prescribed acetaminophen.
- Ambulates with walker, able to bear weight with minimal discomfort.
- No signs of deep vein thrombosis (DVT), no redness or warmth in calf.
Interventions & Care Provided:
- Administered pain medication (acetaminophen 500 mg) as per plan.
- Assisted with mobility exercises, ensuring correct technique to avoid strain.
- Provided education on post-op care, including signs of infection to watch for.
Patient Response:
- Patient reports feeling better with pain under control. Expressed understanding of post-op care instructions.
- Patient performed leg exercises with assistance and tolerated well.
Plan for Follow-up:
- Continue with mobility exercises twice daily.
- Follow-up visit scheduled for January 22, 2026, to reassess mobility and pain levels.
Signature: Nurse Jane Smith, RN
2. Medication Management for Chronic Illness home care nursing note example
Date & Time: January 15, 2026, 11:30 AM
Patient Information: Sarah Lee, DOB 06/12/1945, MRN 789012
Reason for Visit: Medication management for Type 2 diabetes
Clinical Observations:
- Blood sugar reading at 8 AM: 160 mg/dL (slightly elevated).
- No signs of hypo or hyperglycemia observed.
- Vital signs stable: BP 120/78, pulse 76 bpm.
- Patient reports no new symptoms or discomfort related to diabetes.
Interventions & Care Provided:
- Reviewed current medication regimen with patient. Confirmed adherence to prescribed medications.
- Provided education on adjusting meal planning and exercise to better control blood sugar.
- Demonstrated correct use of glucose monitor and reviewed proper techniques for insulin administration.
Patient Response:
- Patient reports understanding of how diet and exercise impact blood sugar.
- Asked questions about adjusting insulin doses; provided clarification.
Plan for Follow-up:
- Monitor blood sugar levels closely, especially after meals.
- Next visit scheduled for January 22, 2026, for follow-up assessment.
Signature: Nurse Laura Green, RN
3. Wound Care and Infection Prevention home health nursing note example
Date & Time: January 15, 2026, 2:00 PM
Patient Information: Mark Turner, DOB 03/29/1972, MRN 345678
Reason for Visit: Wound care for diabetic foot ulcer
Clinical Observations:
- Wound site (left foot) clean and free from drainage.
- Redness around the edges of the ulcer, no signs of pus or fever.
- Patient reports no pain at the site but experiences mild itching.
- Blood sugar level at 9:00 AM: 180 mg/dL.
Interventions & Care Provided:
- Cleansed wound with saline solution, applied new dressing (hydrocolloid).
- Provided education on the importance of keeping the foot elevated and avoiding pressure on the ulcer.
- Reinforced the need for proper foot hygiene and daily inspection for any signs of infection.
Patient Response:
- Patient verbalized understanding of wound care instructions and expressed willingness to follow through with recommended practices.
- No issues reported during the wound dressing change.
Plan for Follow-up:
- Continue daily dressing changes.
- Monitor for signs of infection (increased redness, warmth, or drainage).
- Follow-up visit scheduled for January 18, 2026.
Signature: Nurse Emily Carter, RN
4. Fall Risk Monitoring home care nursing notes
Date & Time: January 16, 2026, 10:00 AM
Patient Information: Betty Williams, DOB 09/15/1935, MRN 567890
Reason for Visit: Fall risk assessment and prevention
Clinical Observations:
- Patient ambulates with a cane, but balance appears slightly unsteady.
- No recent falls reported, but patient reports feeling dizzy when standing up too quickly.
- Vital signs: BP 115/70, pulse 80 bpm, no other abnormalities noted.
Interventions & Care Provided:
- Conducted a fall risk assessment using the Morse Fall Scale, score: 50 (high risk).
- Provided education on safe mobility techniques, including slow transitions when standing.
- Recommended installation of grab bars in the bathroom and a nightlight in the hallway for better visibility at night.
Patient Response:
- Patient expressed concern about falling and agreed to implement recommendations.
- No discomfort reported during the mobility assessment.
Plan for Follow-up:
- Follow-up visit scheduled for January 20, 2026, to reassess fall risk and evaluate home safety improvements.
Signature: Nurse Sarah Thompson, RN
5. Routine Health Check for Elderly Patient home health nursing note example
Date & Time: January 16, 2026, 3:30 PM
Patient Information: Henry Adams, DOB 02/02/1940, MRN 234567
Reason for Visit: Routine health check and monitoring of age-related health issues
Clinical Observations:
- Patient appears well-groomed and in no apparent distress.
- Weight: 170 lbs (no significant change since last visit).
- Blood pressure: 130/80, pulse: 74 bpm, respiration rate: 16 breaths per minute.
- Hearing aids in place, patient reports no difficulty hearing.
Interventions & Care Provided:
- Conducted a routine physical exam, including auscultation of the heart and lungs.
- Provided health education about aging and recommended a balanced diet, regular exercise, and social engagement to improve overall well-being.
Patient Response:
- Patient is satisfied with their current health and shows interest in maintaining independence as they age.
- No immediate concerns raised during the visit.
Plan for Follow-up:
- Next routine visit scheduled for February 16, 2026.
- Encourage patient to stay active and monitor weight and blood pressure regularly.
Signature: Nurse Olivia Johnson, RN
Best Practices for Writing Home Care Nursing Notes
Writing clear and accurate home care nursing notes is an essential skill that ensures the quality of patient care and helps maintain legal and professional standards. Here are some best practices to follow when documenting your notes:
1. Be Factual and Objective
Your nursing notes should be based on facts, not opinions. Focus on what you observed, what actions you took, and how the patient responded. Avoid using subjective or vague terms like “seems better” or “appears fine.” Instead, describe what you saw or did with specific details, such as “patient’s temperature is 98.7°F,” or “patient requested pain medication at 10:00 AM.”
2. Use Clear and Concise Language
Clarity is key. When writing your notes, avoid overly complicated language or long, winding sentences. Stick to short, clear phrases that get straight to the point. This makes it easier for other healthcare professionals to read and understand your documentation quickly.
3. Follow a Consistent Format
Consistency is essential for effective communication. Stick to a standardized format for your notes. This might include headings like “Date/Time,” “Reason for Visit,” “Observations,” and “Plan.” By using a consistent format, you make your notes easier to follow and ensure that all critical information is covered every time.
4. Document in Real-Time
When possible, document your notes as you go. This helps reduce errors and ensures that your observations and actions are recorded while they’re still fresh in your mind. If you’re unable to write in real-time, make sure to write your notes as soon as possible after the visit to ensure accuracy.
5. Use Professional Language
Always use professional, clear, and precise language. Avoid using slang, abbreviations, or jargon unless they are widely understood and accepted in your healthcare setting. This ensures that your notes are universally understood, whether they are being reviewed by another nurse, a physician, or an insurance company.
6. Keep It Brief, but Thorough
Your notes should be thorough enough to provide a complete record of the care provided, but concise enough to avoid unnecessary details. If something is not relevant to the patient’s care, leave it out. However, make sure you include all necessary information, such as interventions, responses, and follow-up plans.
7. Ensure Accuracy
Accuracy is paramount when documenting nursing notes. Double-check that all patient details, medical history, and observations are correct. If there’s any uncertainty about a detail, clarify it with the patient or a colleague before documenting it. Inaccurate documentation can lead to confusion and errors in patient care.
8. Be Timely
Complete your nursing notes as soon as possible after your visit, ideally before you leave the patient’s home. The more time that passes, the more likely it is that important details will be forgotten. Timely documentation also ensures that your notes can be used effectively by other healthcare providers when they need them.
9. Maintain Confidentiality
As a healthcare professional, patient confidentiality is crucial. Ensure that all notes are stored securely, whether they’re on paper or in an electronic health record (EHR) system. Be mindful of HIPAA regulations and avoid discussing sensitive patient information with anyone who is not directly involved in the patient’s care.
Legal & Compliance Considerations for Home Care Nursing Notes
When writing home care nursing notes, it’s not just about documenting the care you’ve provided—it’s also about ensuring that your notes comply with legal and professional standards. Here are some key considerations to keep in mind:
1. Patient Privacy and Confidentiality
Your patients trust you to keep their personal and medical information private, and this trust must be upheld in your documentation. Always ensure that your notes are stored securely, whether in physical or electronic form. Follow HIPAA (Health Insurance Portability and Accountability Act) regulations to protect patient privacy.
If you’re using an electronic health record (EHR) system, make sure it’s HIPAA-compliant and that you follow protocols for access control and data encryption. Never discuss patient details in public places or with people not involved in the patient’s care.
2. Legality of Documentation
Nursing notes serve as legal documents. In cases of disputes, malpractice claims, or audits, your notes may be examined to verify the care that was provided. That’s why it’s crucial that your documentation is accurate, timely, and objective. Any inaccuracies or omissions could potentially be used against you, so always ensure your notes reflect the truth of the situation.
If you’re unsure about what should or shouldn’t be included in your notes, err on the side of caution and document everything that’s relevant to patient care. Include any conversations you’ve had with the patient or their family, and keep detailed records of the care you’ve provided.
3. Compliant with Insurance Requirements
Many home care agencies and insurance companies require that nursing notes meet specific standards in order to justify claims and ensure that patients are receiving necessary care. This means that your notes need to be complete, accurate, and up to date.
Be sure to follow the documentation guidelines set by your employer or healthcare provider. This will ensure that your notes meet the necessary standards for reimbursement and avoid issues with payment delays.
4. Following Your Agency’s Policies and Procedures
Every healthcare organization has its own set of policies and procedures regarding documentation. It’s important to familiarize yourself with these internal guidelines to ensure you’re following the correct process for writing home care nursing notes.
These guidelines might include specific formats, terminology, or documentation requirements that your employer has put in place to maintain consistency across patient records. Adhering to these policies is essential to avoid errors and maintain professional standards.
5. Electronic vs. Paper Notes
Many home care agencies are moving towards electronic documentation, but some still use paper records. Both have their pros and cons.
- Electronic notes are easier to organize, search, and share with other healthcare providers. They can also be more secure if your agency has proper cybersecurity measures in place.
- Paper notes, while less common, are still used in some settings. If you’re documenting on paper, ensure that your notes are legible, organized, and stored securely.
If you’re working with electronic records, make sure you are trained on the system and understand how to properly input, update, and share information. Regardless of the format, maintaining accuracy and confidentiality is key.
Conclusion
In home care nursing, your notes are a vital part of patient care and professional documentation. They not only help you keep track of the care you’ve provided but also serve as a communication tool between healthcare providers, a record for insurance and billing, and, importantly, a legal document.
By following the best practices and ensuring compliance with legal and professional standards, you’ll be able to write notes that are clear, accurate, and reliable. Whether you’re documenting observations, interventions, or patient responses, your notes play a key role in the ongoing care of your patients.
Remember, good documentation is about more than just ticking boxes—it’s about ensuring the best outcomes for your patients and protecting yourself as a healthcare professional. With the right structure and attention to detail, you can make sure that your home care nursing notes serve their purpose and meet the high standards expected in the healthcare field.
As you continue to build your skills in home care nursing, keep these best practices in mind. You’ll find that strong documentation makes your job easier, improves patient care, and provides peace of mind knowing that everything is accurately recorded.
Frequently Asked Questions (FAQs)
Q1: Can I use abbreviations in home care nursing notes?
Yes, but only those approved by your agency or widely recognized in clinical practice. Avoid facility-specific shorthand when sharing notes outside the organization.
Q2: How long should a home care nursing note be?
Most fall between 150–250 words—long enough to capture all essential details, but without unrelated or repetitive content.
Q3: What’s the biggest difference between home care nursing notes and hospital progress notes?
Home care notes often include more caregiver interactions, patient teaching, and environmental observations since the setting is the patient’s home.
Q4: Can nursing students use these examples in assignments?
Yes—just ensure patient confidentiality and adapt examples to your case scenario.
Q5: Are these notes legally binding?
Absolutely. Once signed, they become part of the permanent health record and can be used in audits, insurance reviews, and court proceedings.

