Accurate nursing notes are at the heart of safe, consistent patient care. They capture not just what you did, but how the patient responded — creating a clear picture that guides everyone involved in treatment. Whether you’re updating an electronic health record or jotting down observations after rounds, strong documentation shows your attention to detail and professionalism.
Good nursing notes go beyond basic record-keeping. They demonstrate critical thinking, highlight timely interventions, and protect both you and your patients. When done well, documentation becomes a communication tool that ensures every team member understands what happened and what needs to happen next.
This guide shares real examples of good nursing notes, along with ready-to-use templates and charting tips designed to make documentation faster, clearer, and more effective — no matter your unit or specialty.
And you’re doing it on top of work and family life. That’s exactly why we exist — to give you back your evenings, your weekends, and your peace of mind. We’ll take care of the writing. You take care of you.
What Makes a Nursing Note “Good”?
A good nursing note tells a clear, factual story that anyone on the care team can understand — even days later. It connects the dots between what you observed, what you did, and how the patient responded. When written well, your notes become a reliable timeline of care that protects both the patient and you.
Qualities of good Nursing Notes
Every strong nursing note shares five traits:
- Accurate – Record exact times, measurements, and patient statements. Avoid guesses or vague language.
- Objective – Stick to observable facts. Describe behavior, not emotion.
- Clear – Write in simple, professional language, as if you’re briefing a colleague.
- Timely – Chart as soon as possible after providing care to ensure accuracy.
- Complete – Include the full nursing process: assessment, intervention, patient response, and signature.
Together, these elements turn a routine note into a professional record of accountability and care.
Types of Nursing Notes (and When to Use Each)
Not every patient situation fits the same documentation style. That’s why nurses use different note formats — each with its own structure, strengths, and best use cases. Understanding when to use each type saves time, reduces confusion, and keeps your charting consistent across shifts.
| Format | Best For | Structure | Strength | Watch-Outs |
| Narrative | General shift notes, post-op care, ongoing observations | Freeform paragraph | Flexible, easy to read | Can be lengthy or miss key data |
| SOAP / SOAPIE / SOAPIER | Problem-focused notes (e.g., acute symptoms, wound care, behavioral issues) | Subjective, Objective, Assessment, Plan, [Intervention, Evaluation, Revision] | Structured, promotes clinical reasoning | Can feel repetitive or rigid |
| PIE | Daily nursing process and care plans | Problem, Intervention, Evaluation | Directly links to nursing diagnoses | Lacks “Assessment” detail |
| DAR (Focus) | Quick, focused charting (behavioral or symptom-based) | Data, Action, Response | Time-efficient, easy to adapt | May miss broader context |
| CBE (Charting by Exception) | Routine care with defined standards | Only records deviations from normal | Saves time, highlights abnormalities fast | Can overlook subtle changes |
Each format offers a slightly different lens for documenting care. The goal isn’t to memorize templates — it’s to choose the one that tells the clearest story for the patient situation you’re facing.
Nursing Note Examples by Setting
Below are Good nursing note examples in multiple charting styles — SOAPIE, PIE, DAR, and Narrative — each tailored to a different care environment. You’ll see what poor documentation looks like, followed by a strong, time-stamped version that meets professional and legal standards.
1. Med-Surg / Acute Care (SOAPIE Note)
Bad Example:
“Patient complained of pain. Gave pain meds. Feeling better.”
This note is incomplete — it lacks time stamps, assessment data, intervention details, and patient response.
Good Example (SOAPIE):
Patient: Robert K.
Date: June 2, 2025
07:32: Patient alert and oriented ×3. Reports incisional pain rated 6/10 after ambulating 40 ft with assistance. Dressing dry and intact. (Subjective)
Incision clean, no redness or drainage. Vitals stable: BP 118/80, HR 84, RR 18, SpO₂ 97% RA. (Objective)
Post-operative pain related to surgical incision. (Assessment)
Plan to administer analgesic and encourage use of incentive spirometer. (Plan)
07:45: Administered oxycodone 5 mg PO per order. Encouraged deep breathing and coughing. (Intervention)
08:15: Pain reassessed — patient rates pain 3/10 and reports comfort. Demonstrated proper IS use to 1200 mL. (Evaluation)
Why This Works:
This SOAPIE note provides a complete care sequence with measurable outcomes, legal protection, and clear continuity for the next nurse.
2. Pediatric / Home Health (DAR Note)
Bad Example:
“Taught mom about meds. She said okay.”
This note fails to show what was taught, how it was taught, or whether understanding was verified.
Good Example (DAR):
Patient: Mia S.
Date: April 18, 2025
14:05: Child observed using inhaler incorrectly; mother reports missed doses during school hours. (Data)
Demonstrated correct spacer technique and had child perform return demonstration twice successfully. Reviewed dosage schedule and reinforced adherence with parent. (Action)
Parent verbalized understanding and accurately repeated instructions. Plan to review technique next visit. (Response)
Why This Works:
This DAR note shows education, teach-back, and engagement of both child and caregiver — covering the essential elements of home health documentation.
3. Mental Health / Psychiatric Unit (PIE Note)
Bad Example:
“Patient anxious, gave meds, seems okay now.”
This note lacks objectivity, measurable outcomes, and timeline clarity — key issues in mental health documentation.
Good Example (PIE):
Patient: Daniel T.
Date: March 8, 2025
10:20: Patient pacing and expressing frustration, stating, “I can’t calm down.” (Problem)
Provided quiet environment, encouraged deep breathing, and administered lorazepam 1 mg PO at 10:25 per PRN order. (Intervention)
At 10:50, patient seated calmly, states, “I feel better now.” No further agitation observed. (Evaluation)
Why This Works:
This PIE note uses objective language, specific timing, and measurable response — ensuring accurate behavioral tracking and continuity of care.
4. Long-Term Care / Geriatrics (Narrative Note)
Bad Example:
“Resident almost fell but is fine. No injuries.”
This entry is vague and misses important safety actions, education, and follow-up details.
Good Example (Narrative):
Patient: Ellen M.
Date: August 15, 2025
20:25: Resident found seated at bedside, states she “almost slipped while reaching for slippers.” No injuries noted. Assisted safely to chair. Vitals WNL. Educated on use of call light before ambulating. Fall mat in place, bed alarm activated. Will monitor Q2H for safety.
Why This Works:
This narrative note is concise yet complete — documenting patient statement, assessment, intervention, education, and plan, which protects both the nurse and facility legally.
5. Emergency Department (SOAPIE Note)
Bad Example:
“Patient came in with chest pain. Doctor notified. Given meds.”
This lacks clinical data, times, interventions, and outcome — all crucial in emergency care.
Good Example (SOAPIE):
Patient: Adam L.
Date: May 4, 2025
07:58: Reports mid-sternal chest pressure 7/10 since 0700. (Subjective)
BP 162/94, HR 110, SpO₂ 95% RA. ECG performed 0802 showing sinus tachycardia. (Objective)
Possible acute coronary syndrome. (Assessment)
Plan to administer aspirin and oxygen, notify provider. (Plan)
08:05: Administered aspirin 325 mg PO and O₂ 2 L via nasal cannula. IV line established. (Intervention)
08:20: Patient reports pain decreased to 3/10. HR 96, BP 148/86. Provider updated; patient admitted for observation. (Evaluation/Revision)
Why This Works:
This SOAPIE note includes complete assessment, interventions, response, and escalation — the level of precision expected in emergency nursing.
Quick Checklist Before Submitting a Note
Before you hit “submit” or sign off, take a few seconds to run through this quick safety checklist:
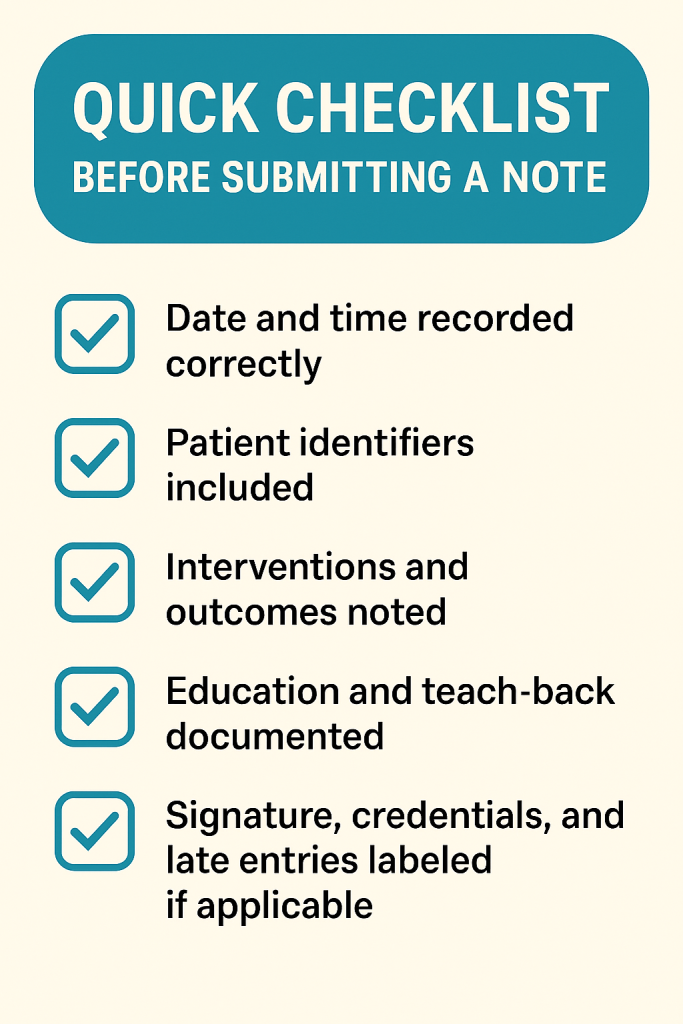
A good rule of thumb: if another nurse could safely take over care after reading your note, you’ve written it well.
Common Mistakes to Avoid
Even experienced nurses can make charting mistakes when the unit is busy. Fatigue, multitasking, or time pressure can easily lead to vague or incomplete notes. But small errors in documentation can create big risks — from legal issues to care gaps. Here’s what to watch for and how to fix it.
1. Using Vague or Subjective Language
Avoid words like “doing better” or “slept well.” These don’t communicate anything measurable.
Instead: use data and specifics.
Example: “Pain reduced from 8/10 to 3/10 after 5 mg oxycodone.”
2. Adding Emotion or Judgment
Terms like “lazy,” “uncooperative,” or “angry” can sound biased. Describe behavior, not attitude.
Example: “Patient declined bath, stating, ‘I’m too tired today.’”
3. Copy-Pasting Previous Entries
It’s tempting when you’re short on time, but repeating yesterday’s note means today’s care might not be accurately documented. Always update with current findings.
4. Leaving Blanks or Skipping Responses
A missing patient response can make your note incomplete. Always document how the patient reacted to your intervention — even if the response was no change.
5. Forgetting Education and Communication
Document every call to the provider, every teaching moment, and every refusal. These are key parts of patient safety and continuity of care.
💡 Pro Tip: Before signing off, ask yourself —
“Could someone else safely continue care based only on this note?”
If not, add the missing detail before you clock out.
Documenting Abnormal Findings (Mini Guide)
Abnormal findings are the moments when your documentation matters most. A sudden fever, a new confusion episode, or a change in wound drainage can all signal something serious. In these moments, your note becomes a clinical and legal lifeline — guiding the next nurse, informing the provider, and protecting the patient.
Common Abnormal Situations
Here are frequent scenarios that call for detailed, factual nursing documentation:
- Neurological changes: confusion, slurred speech, unequal pupils
- Wound changes: redness, swelling, drainage, foul odor
- Vital sign abnormalities: fever, hypotension, tachycardia
- Behavioral changes: agitation, withdrawal, hallucinations
- Adverse reactions: rash, nausea, medication refusal
- Safety events: falls, near-misses, dislodged IVs or tubes
Each situation demands a clear and complete record — one that answers what happened, what was done, and how the patient responded.
Step-by-Step: How to Document Abnormal Findings
- Describe the abnormality clearly.
Use precise, objective details.
Example: “Temp 102.4°F, flushed skin, shivering” — not “patient feverish.” - Record immediate actions.
Include what you did right away — repositioning, assessment, medication, or call for help. - Document who was notified and when.
Add provider names and exact times. Timeliness shows accountability. - Include new orders or interventions.
Record treatment, monitoring plans, or tests ordered. - Note the patient’s response.
Always follow up with results or observed changes. - End with next steps.
“Will continue to monitor” is fine, but be specific: “Will monitor Q1H for changes.”
Example: Abnormal Finding – New Onset Confusion
Scenario:
Elderly patient becomes disoriented and agitated after lunch.
Example (Narrative Note):
1330 – Patient oriented ×1, repeatedly asking, “Where am I?” Attempted to get out of bed unassisted. Assisted back to bed; side rails up ×2; call light within reach. BP 168/92, Temp 101.8°F, HR 104. Provider notified 1335; order received for UA and Tylenol 650 mg PO. Med administered 1345. At 1415, patient calmer, oriented ×2. Will monitor Q1H.
Why It Works:
- Includes complete timeline and clinical reasoning.
- Documents assessment, action, and response.
- Meets safety, legal, and handoff standards.
Pro Tips for Abnormal Documentation
- Chart immediately. Delays can make your record appear unreliable.
- Avoid assumptions. Describe, don’t diagnose (“patient likely infected”).
- Use approved abbreviations only. Keeps your notes clear and compliant.
- Record every notification. Always include names and times.
- Check timestamps twice. Accuracy matters during audits and investigations.
When things go wrong, your words tell the story. The best nursing notes examples for abnormal findings don’t just describe — they show action, communication, and follow-up.
The Do’s and Don’ts of Good Nursing Notes
Your nursing notes aren’t just communication tools — they’re legal records. Every line you write can protect your license, your patient, and your integrity. Think of documentation as your written testimony: factual, complete, and professional.
Documentation Do’s
- Chart promptly and accurately.
Record care immediately after providing it. If a late entry is needed, clearly label it with the actual time of the event and the time of documentation. - Use only approved abbreviations.
Each facility has its own list. When in doubt, write out the full term to avoid confusion during emergencies. - Stay objective — not emotional.
Describe what you observe, not what you feel.
- ✅ “Patient pacing and shouting, fists clenched.”
- ❌ “Patient angry and uncooperative.”
- ✅ “Patient pacing and shouting, fists clenched.”
- Document patient education and understanding.
Note what was taught, how it was delivered (verbal, demo, handout), and how the patient or caregiver responded. - Sign every entry.
Always include your full name, credentials, date, and time.
Example: Jane Doe, RN — 10/13/25, 1430 - Follow facility policy for corrections.
Draw a single line through the error, write “error,” and initial it. Never erase, delete, or overwrite — transparency builds trust.
Documentation Don’ts
- ❌ Don’t leave blanks — someone could fill them in later.
- ❌ Don’t chart ahead — only record what’s already done.
- ❌ Don’t copy-paste — duplication creates confusion and liability.
- ❌ Don’t use vague terms like “appears stable” or “doing fine.”
- ❌ Don’t include retaliatory or emotional comments (e.g., “patient difficult again”). Stay factual, not personal.
Templates, Tools, and Quick References
Great documentation isn’t just about what you write — it’s about having the right tools to do it efficiently. The templates below are designed to help you chart faster, stay organized, and ensure nothing important slips through.
1. SOAP Note Template
When to Use:
For focused, problem-based charting — ideal for wound care, chest pain, medication reactions, or acute symptoms.
Structure:
- S (Subjective): What the patient says.
- O (Objective): What you observe — vitals, findings, measurements.
- A (Assessment): Your clinical interpretation.
- P (Plan): Planned interventions or next steps.
- I (Intervention): What you actually did.
- E (Evaluation): Patient’s response.
- R (Revision): Any updates or changes to the care plan.
Example – Respiratory Distress:
S: “I’m feeling short of breath again.”
O: RR 26, SpO₂ 91% RA, bilateral wheezes noted.
A: Impaired gas exchange.
P: Administer albuterol and monitor SpO₂.
I: Treatment given 1115.
E: SpO₂ improved to 97%, RR 20, breathing easier.
R: Continue monitoring every 2 hours.
2. PIE Note Template
When to Use:
Ideal for care plans linked to nursing diagnoses or ongoing interventions.
Structure:
- P (Problem): Identify the nursing diagnosis or issue.
- I (Intervention): Record what care you provided.
- E (Evaluation): Describe the patient’s response.
Example – Post-Op Pain:
P: Acute pain related to surgical incision, rated 7/10.
I: Administered oxycodone 5 mg PO at 0900.
E: Pain reduced to 3/10 at 0930; resting comfortably.
3. Narrative Note Template
When to Use:
For shift summaries, ongoing assessments, or flexible documentation when structure isn’t required.
What to Include:
- Time and date
- Patient assessment
- Interventions performed
- Patient response
- Follow-up or plan
Example – Nausea:
0700 – Alert and oriented ×3. Reports nausea without vomiting. Given ondansetron 4 mg PO. At 0730, nausea resolved; tolerated oral fluids. Will monitor for recurrence.
4. DAR (Focus) Note Template
When to Use:
For short, focused charting on a specific concern like pain, anxiety, or new symptoms.
Structure:
- D (Data): Objective and subjective findings.
- A (Action): What you did, taught, or advised.
- R (Response): Patient’s reaction or outcome.
Example – Pre-Op Anxiety:
D: Patient tearful and restless before surgery.
A: Explained procedure, answered questions, encouraged deep breathing.
R: Patient verbalized understanding, appeared calmer, and cooperated with pre-op prep.
Abbreviation Cheat Sheet
A few of the most common, facility-approved abbreviations used in nursing documentation:
| Abbreviation | Meaning |
| BP | Blood Pressure |
| HR | Heart Rate |
| SpO₂ | Oxygen Saturation |
| A&O ×3 | Alert and Oriented to person, place, time |
| PRN | As Needed |
| WNL | Within Normal Limits |
| Q2H | Every 2 Hours |
| PO | By Mouth |
| N/V | Nausea/Vomiting |
| C/O | Complains Of |
Shift Note Checklist
Before you clock out, do a quick self-audit:
✅ Time and date recorded correctly
✅ Objective findings clearly stated
✅ Interventions and patient responses documented
✅ Education and understanding noted
✅ Provider notification (name + time) included
✅ Follow-up plan documented
✅ Signature and credentials present
Why Templates Matter
Templates don’t make your charting robotic — they make it reliable.
They help you stay consistent, ensure completeness, and tell the patient’s story in a clear, professional way. Over time, this structure becomes second nature, helping you chart faster and more confidently.
The best nursing documentation examples combine structure and story — a balance that makes your care easy to understand at a glance.
Final Thoughts
Good nursing notes are more than a task on your checklist — they’re your professional signature at the end of every shift. Each entry you write tells a story of observation, judgment, and compassion. When done well, it builds trust, supports clinical decisions, and protects both you and your patient.
The best nursing documentation isn’t about long paragraphs or perfect grammar — it’s about clarity. It shows what happened, what you did, and how the patient responded. Whether you’re writing a SOAP note for chest pain, a PIE note for wound care, or a narrative report at the end of your shift, your purpose stays the same: to make care traceable, safe, and complete.
Start small:
- Use the templates in this guide.
- Review your notes before signing.
- Practice turning real patient moments into concise, factual statements.
With time, charting becomes second nature — quick, confident, and accurate.
And when you look back over your notes at the end of a long week, you’ll see more than just text on a screen.
You’ll see the story of safe, meaningful nursing care — told one good note at a time.
Frequently Asked Questions
Nursing documentation can feel confusing at first — especially when every note type seems to have its own rules. Below are common questions nurses and students ask about writing clear, accurate, and professional notes.
1. How long should a nursing note be?
Long enough to tell the full story — no longer.
A good nursing note captures the essentials: assessment, intervention, response, and plan. Most shift notes are 3–6 concise lines per event. Brevity is good, but clarity always comes first.
Remember: If it isn’t documented, it didn’t happen.
2. What’s the difference between SOAP, PIE, and DAR notes?
| Format | Focus | Best Used For |
| SOAP / SOAPIE | Problem-oriented and analytical | When detailed clinical reasoning is needed (e.g., pain, infection, injury) |
| PIE | Nursing process-based (Problem, Intervention, Evaluation) | For ongoing care plans and nursing diagnoses |
| DAR (Focus) | Symptom- or behavior-based | For short, focused notes like anxiety, refusal, or agitation |
Each style has its strength: SOAP builds logic, PIE connects to diagnoses, and DAR keeps documentation concise.
3. How do I document a patient refusal?
Be factual and show follow-up.
Example:
0900 – Patient refused insulin dose, stating, “I don’t need it today.” Educated on purpose and risk of skipping dose. Provider notified; will continue to monitor.
Avoid judgmental language or assumptions. Your note should show that you informed, educated, and escalated appropriately.
4. Can I use abbreviations or shortcuts?
Yes — but only those approved by your facility.
Unapproved abbreviations (like “U” for units or “QD” for daily) can lead to confusion or medication errors. When unsure, write it out.
5. Is it okay to copy and paste previous notes?
Not recommended.
Copy-pasting can carry over outdated or incorrect data. Instead, use templates or smart phrases and customize them for the current shift. Every patient encounter deserves a fresh, accurate note.
6. What happens if I forget to chart something important?
Add a late entry as soon as possible. Label it clearly with both the current date/time and the time the event occurred.
Example:
Late Entry (10/13/25 1400): At 0830, patient reported dizziness; BP 88/54. Provider notified; 250 mL NS bolus started.
Never backdate — transparency protects you legally and ethically.
7. How short can a note be with Charting by Exception (CBE)?
CBE allows you to record only deviations from normal, but your note must still ensure continuity of care.
Example:
1500 – Temp 100.6°F. Provider notified; acetaminophen 650 mg PO given. Will recheck in 1 hour.
Short is fine. Incomplete is not.
8. How can I chart faster without missing details?
- Chart in real time — not at the end of the shift.
- Use templates or checklists (like the ones above).
- Create “charting phrases” for common situations (pain, wound care, education).
- Always review before signing.
Efficiency improves with routine, not shortcuts.
9. Should I document patient education?
Absolutely — and every time.
Education notes serve as legal proof that teaching occurred and that the patient understood. Document what you taught, how you taught it (verbal, demo, handout), and how the patient or caregiver responded.
10. What’s the single best rule for good nursing notes?
Be clear, factual, and complete.
If another nurse can safely take over after reading your note, you’ve done your job.
Good nursing documentation is not about fancy language — it’s about professional, honest communication that reflects quality care.

