Every nurse knows that small actions can make a big difference. Washing your hands before patient care. Checking a fall-risk score. Asking a patient to repeat back discharge instructions. These moments may feel routine, but they’re backed by research that saves lives. That’s the heart of evidence-based practice.
In this article, we’ll go beyond simple definitions and look at nursing evidence-based practice examples — and much more. You’ll get a refresher on the five steps of EBP, see 15 real scenarios you can apply right away, and learn how to find and appraise the right evidence. We’ll also explore the benefits of EBP, common challenges nurses face, and practical tips for overcoming them. To wrap up, you’ll find FAQs and strategies you can put into practice immediately.
You’re juggling work, classes, and family, and still finding the energy to care for everyone else. That kind of strength deserves support, not burnout. Let our nursing writers step in when life gets too full so you can finally breathe.
The 5 Steps of Evidence-Based Practice in Nursing
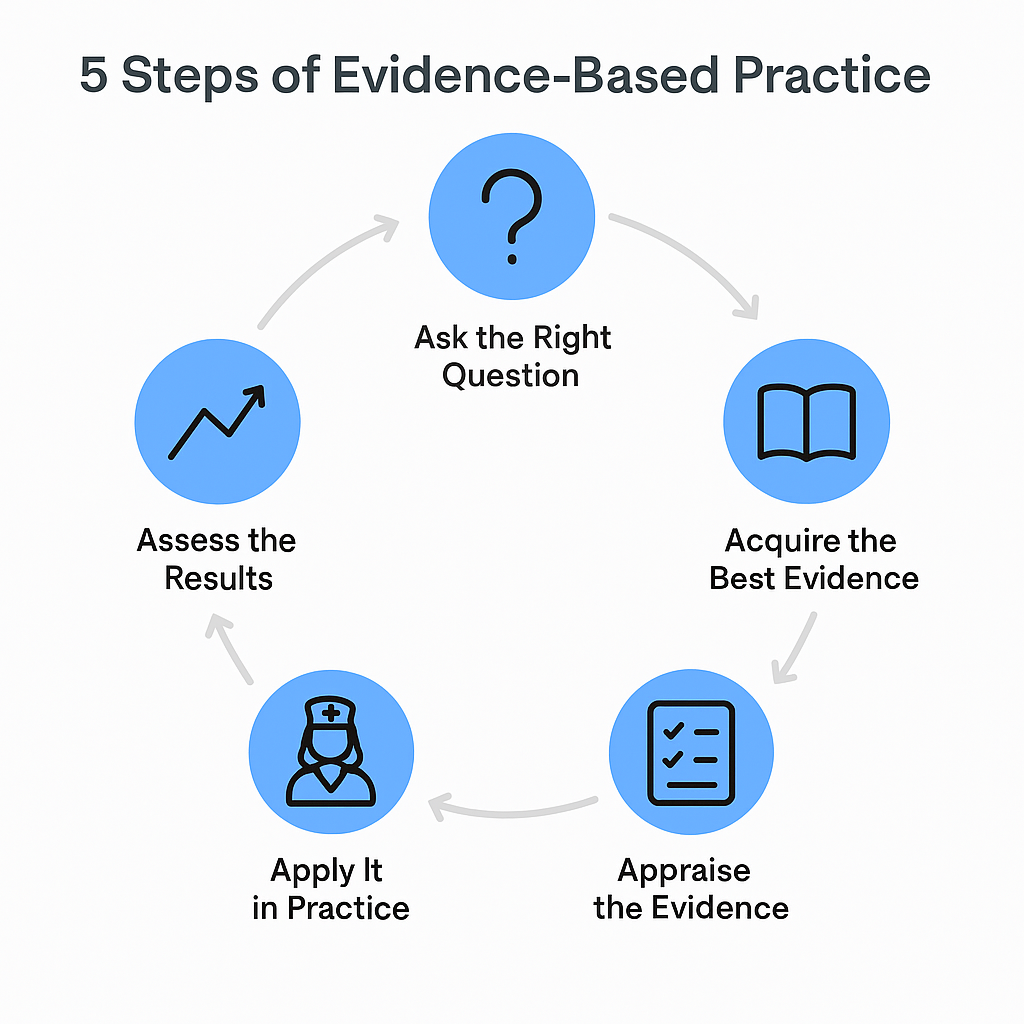
Evidence-based practice (EBP) is more than a checklist — it’s a cycle that nurses use to connect research with patient care. By following these five steps, you make sure your decisions are grounded in evidence, shaped by your clinical judgment, and respectful of patient values.
1. Ask the Right Question
EBP starts with curiosity. Nurses see problems every day: Why are falls so common on night shifts? Is this dressing the best choice for preventing pressure injuries? Turning these observations into structured clinical questions is the first step.
The PICOT format helps:
- P – Patient or problem
- I – Intervention
- C – Comparison
- O – Outcome
- T – Time (optional)
📌 Example: In post-op patients (P), does early ambulation (I) compared to bed rest (C) reduce pneumonia (O) in the first 48 hours (T)?
2. Acquire the Best Evidence
Once you have a question, you need answers. Nurses don’t have hours to search through journals, so the smartest move is using trusted sources:
- Clinical guidelines from bodies like ANA, CDC, WHO
- Hospital protocols and toolkits (AHRQ, AACN, WOCN)
- Databases like CINAHL, PubMed, Cochrane
3. Appraise the Evidence
Not all research is equal. A blog post is not the same as a systematic review. Nurses need to weigh:
- Currency – Was it published in the last 5 years?
- Credibility – Is it peer-reviewed or from a trusted health organization?
- Relevance – Does it fit your patient population and resources?
- Strength – Systematic reviews and RCTs sit higher on the evidence pyramid than case studies.
4. Apply It in Practice
This is where theory meets the bedside. Nurses adapt evidence to their unit’s workflow and patient needs. For example:
- Using the Morse Fall Scale to guide safety plans
- Following a nurse-driven Foley removal protocol to prevent CAUTIs
- Teaching a patient with heart failure using the teach-back method
Evidence alone doesn’t change care — your clinical judgment and the patient’s values shape how it’s applied.
5. Assess the Results
The cycle doesn’t end with application. Nurses evaluate whether the intervention worked:
- Did falls decrease on the unit?
- Was the patient able to explain their medication schedule?
- Did infection rates drop after starting the bundle?
This step closes the loop and often sparks new questions — restarting the EBP process.
Why it matters: By using these five steps, nurses transform routine tasks into intentional actions backed by science. It ensures care is consistent, effective, and trusted — not just habit or tradition.
15 Nursing Evidence-Based Practice Examples
These aren’t theories — they’re practices you see in hospitals, clinics, and long-term care every day. Each example comes with a quick scenario, what the evidence says, and how you might chart it.
1. Hand Hygiene to Prevent Infections
- Scenario: A nurse washes hands before touching supplies or the patient.
- Evidence: Consistent hand hygiene can cut hospital infections by up to 40%.
- Documentation: “Hand hygiene done before and after patient contact.”
📷 Suggested image: Nurse using sanitizer dispenser at the bedside.
2. Nurse-Driven Foley Removal (CAUTI Prevention)
- Scenario: The nurse reviews a patient’s Foley catheter during rounds and removes it when no longer needed.
- Evidence: Nurse-led Foley removal lowers CAUTI rates by 30–50%.
- Documentation: “Catheter removed per protocol; post-void residual checked.”
3. Central Line Bundle (CLABSI Prevention)
- Scenario: A nurse scrubs the hub for 15 seconds before central line access.
- Evidence: Bundles with hand hygiene, chlorhexidine prep, and daily reviews cut infection risk.
- Documentation: “Central line accessed with sterile technique; hub scrubbed.”
4. Ventilator-Associated Pneumonia (VAP) Bundle
- Scenario: ICU nurse elevates the head of bed to 35° and gives oral care every 4 hours.
- Evidence: VAP bundles reduce pneumonia in ventilated patients.
- Documentation: “HOB 35°; oral care with CHG completed q4h.”
5. Sepsis Bundle
- Scenario: Within an hour of sepsis recognition, the nurse collects blood cultures and starts fluids.
- Evidence: Early sepsis bundles lower death rates.
- Documentation: “Blood cultures sent; antibiotics started within 60 minutes.”
6. Pressure Injury Prevention (SSKIN + Braden Scale)
- Scenario: Nurse scores patient with Braden Scale, applies foam dressings, and repositions every 2 hours.
- Evidence: Braden + SSKIN bundle prevents ulcers.
- Documentation: “Braden 14; repositioned q2h; sacral foam applied.”
7. Falls Prevention with Morse Fall Scale
- Scenario: A high-risk patient (Morse 55) gets a bed alarm and non-slip socks.
- Evidence: Morse-guided precautions lower falls.
- Documentation: “Morse 55; fall precautions in place; hourly rounds.”
8. ABCDEF Bundle in the ICU
- Scenario: Team reviews pain, sedation, delirium screen, mobility, and family involvement.
- Evidence: ABCDEF bundle reduces delirium and improves survival.
- Documentation: “CAM-ICU negative; mobilized to chair; family included in plan.”
9. Multimodal Pain Management
- Scenario: Nurse offers acetaminophen and a heat pack before opioids.
- Evidence: Combining meds with non-drug options improves control, reduces opioid use.
- Documentation: “Pain 7/10; Tylenol + heat applied; reassess in 30 min.”
10. Early Mobility Protocol
- Scenario: Post-op patient sits in chair for breakfast on day one.
- Evidence: Early mobility cuts pneumonia, clots, and delirium.
- Documentation: “Ambulated 40m with assist x1; tolerated well.”
11. Teach-Back for Discharge Education
- Scenario: Heart failure patient repeats back daily weight and fluid restriction steps.
- Evidence: Teach-back improves understanding, lowers readmissions.
- Documentation: “Patient verbalized self-care steps using teach-back.”
12. Medication Reconciliation
- Scenario: Nurse reviews meds on admission and spots duplicate anticoagulant.
- Evidence: Accurate reconciliation prevents medication errors.
- Documentation: “Home meds reviewed; duplicate anticoagulant stopped.”
13. COPD Oxygen Titration
- Scenario: Patient with COPD kept at 88–92% oxygen saturation.
- Evidence: Controlled oxygen prevents CO₂ retention.
- Documentation: “O₂ titrated to sats 90–92%; patient monitored.”
14. Pediatric Blood Pressure Technique
- Scenario: Nurse uses correct cuff size, confirms high BP with auscultation.
- Evidence: Auscultation is more accurate than oscillometric alone.
- Documentation: “BP 118/76 by auscultation; correct cuff size used.”
15. Hourly Rounding & SBAR Handoffs
- Scenario: Nurse uses SBAR during handoff and checks on patient hourly.
- Evidence: Structured rounding improves safety and prevents missed care.
- Documentation: “SBAR handoff done; patient concerns addressed during rounds.”
How to Find and Appraise Evidence in Nursing
Evidence-based practice works best when you know where to look. Nurses don’t have hours to read journals, so here are quick ways to find and judge reliable evidence.
Where to Find Reliable Evidence
- Clinical guidelines: ANA, CDC, WHO publish step-by-step recommendations.
- Databases: CINAHL, PubMed, and Cochrane Library hold peer-reviewed studies.
- Hospital resources: Many facilities use UpToDate or in-house protocols.
- Nursing toolkits: AHRQ or specialty groups (AACN for ICU, WOCN for wound care).
Quick Appraisal Checklist
Ask yourself:
- Is it current? (Prefer within 5 years)
- Is it credible? (Peer-reviewed or from a health authority)
- Is it relevant? (Fits your patients and setting)
- Is it strong? (Systematic reviews > expert opinion)
- Does it fit patient values?
Pro Tip: Pyramid of Evidence
- Top: Systematic reviews, meta-analyses, guidelines
- Middle: RCTs, cohort studies
- Bottom: Case studies, expert opinion
The higher up you go, the stronger the evidence. But even expert advice can help when stronger research isn’t available.
EBP isn’t about hours in a library. It’s about using the best shortcuts, grabbing strong evidence, and turning it into safe care at the bedside.
Benefits of Evidence-Based Practice in Nursing
Evidence-based practice (EBP) is more than a trend. It shapes patients’ lives, builds nurse confidence, and strengthens health systems.
Better Patient Outcomes
- Fewer complications: Bundles for CAUTI, CLABSI, and VAP lower infections by up to 40%.
- Safer care: Tools like the Braden and Morse Scales prevent harm.
- Faster recovery: Early mobility and multimodal pain plans help patients heal sooner.
Stronger Nurse Confidence and Growth
- EBP supports critical thinking and autonomy.
- Nurses feel empowered when choices are backed by research.
- Sharing EBP wins boosts team morale.
Organizational Payoff
- Cost savings: Preventing infections and readmissions lowers expenses.
- Accreditation: Magnet hospitals highlight EBP as a marker of excellence.
- Quality scores: Hospitals using EBP often perform better on safety metrics.
Building Patient Trust
Patients notice when care is consistent and backed by evidence. When you explain, “We do this because research shows it works,” you strengthen trust and relationships.
EBP is not extra work. It’s smarter work.
Challenges and Practical Tips for Nurses
EBP sounds simple, but real-life barriers make it harder. Knowing these challenges — and having tools to solve them — makes all the difference.
Common Challenges
- Time pressure: Heavy workloads leave little time for research.
- Access issues: Not every nurse has journal or database access.
- Resistance to change: Some staff prefer old habits.
- Confidence gap: New nurses may feel unsure about evaluating studies.
- Resource limits: Smaller facilities may lack staff or funding.
Practical Tips
- Use quick sources: Bookmark CDC, ANA, and AHRQ guidelines.
- Lean on your team: Shared governance councils can review evidence together.
- Start small: Try one intervention (like hourly rounding) before bigger changes.
- Ask educators: Clinical specialists and educators can guide you.
- Document well: Connect EBP actions to charting so results are visible.
Mindset Shift
EBP isn’t replacing experience with research. It’s combining your judgment, patient values, and the best available evidence.
FAQs on Nursing Evidence-Based Practice Examples
What is a simple example of EBP in nursing?
Hand hygiene. Research shows consistent hand washing and sanitizer use can cut hospital infections by nearly half. It’s quick, cheap, and effective.
What are the 5 steps of evidence-based practice in nursing?
- Ask a focused question (often with PICOT).
- Acquire the best evidence.
- Appraise the quality and relevance.
- Apply it with patient input.
- Assess the results and adjust.
Which tools do nurses use as part of EBP?
- Morse Fall Scale – fall risk assessment.
- Braden Scale – pressure injury risk.
- Teach-back method – patient education.
- Bundles – CAUTI, CLABSI, VAP, ABCDEF.
How does EBP improve patient safety?
It reduces errors and prevents complications. For example, nurse-driven Foley removal lowers infections, and early mobility decreases pneumonia and clots.
Is EBP only for big hospitals?
No. Small clinics and facilities benefit too. Even one practice, like teach-back during discharge, can improve safety and understanding.
How can nursing students practice EBP?
Start small:
- Write PICOT questions.
- Review guidelines.
- Try small projects during clinicals (e.g., hourly rounding, tracking fall scores).
Conclusion
Nursing evidence-based practice examples prove that the choices you make each shift matter. By combining research, clinical skill, and patient values, you build trust, improve safety, and grow as a professional.
You don’t need to change everything at once. Choose one EBP tool or bundle, try it, and see how it transforms care. Evidence doesn’t sit in journals — it lives in your practice.

