Shift change is one of the most critical times in patient care. During this transition, responsibility moves from one nurse to another, and the accuracy of information exchanged can directly affect patient safety and continuity of care.
Bedside shift report is a method designed to bridge communication gaps during this handoff. Instead of exchanging the report in a separate room, both nurses review key information at the patient’s bedside, allowing for real-time verification of the patient’s condition, environment, and immediate priorities.
While this practice is becoming more common, its success depends on proper implementation. Without structure, a bedside report can feel inefficient or incomplete. With clear expectations and practical tools, it can improve accuracy, accountability, and patient involvement.
This guide will explain what bedside shift report is, why it’s important, and how to implement it effectively using checklists, templates, and examples. It also covers common challenges and ways to manage them in real-world settings.
What Is Bedside Shift Report?
Bedside shift report is a handoff process in which outgoing and incoming nurses conduct part of the report at the patient’s bedside, rather than away from the room. Unlike other end of shift reports which do not require the patient to be present
During bedside shift report, both nurses:
- Review the patient’s current condition
- Confirm essential clinical information
- Visually assess the patient and the care environment
- Clarify immediate plans and safety concerns
The patient may be included in the discussion when appropriate. However, a bedside report doesn’t require all information to be shared in front of the patient. Sensitive details, complex histories, or private concerns are often discussed before entering the room, with the bedside portion focused on current status and priorities.
Many units use structured communication tools like SBAR (Situation, Background, Assessment, Recommendation) to guide the report. This approach helps organize the information, while the bedside setting allows nurses to verify its accuracy and reduce assumptions.
Why Is Bedside Shift Report Important in Nursing?
Bedside shift report addresses a significant source of error in healthcare: breakdowns in communication during transitions of care.
Traditional handoff methods rely heavily on verbal summaries or written documentation. When information is incomplete or misunderstood, the incoming nurse may begin the shift without a clear understanding of the patient’s status. Bedside shift report adds an extra layer of verification by allowing both nurses to directly observe the patient and the care environment.
This practice also promotes professional accountability. Conducting a report at the bedside clarifies responsibility for ongoing care and reduces ambiguity about the patient’s condition, equipment, and immediate risks.
From a nursing perspective, bedside shift report aligns with broader priorities:
- Safer handoffs
- Clear communication
- Patient-centered care
- Reduction of preventable errors
Its primary purpose is not to replace clinical judgment, but to strengthen the reliability of information passed from one nurse to the next.
Benefits of Bedside Shift Report in Nursing Practice
When implemented consistently and with clear structure, a bedside shift report offers several practical advantages. These benefits directly relate to how information is transferred, how risks are identified, and how responsibility is handed off between shifts.
The main benefits fall into three areas: patient safety, nurse accountability, and patient satisfaction.
Bedside Shift Report and Patient Safety
Patient safety is the most frequently cited benefit of bedside shift report, and for good reason. Conducting a report at the bedside allows nurses to verify critical information instead of relying on memory or secondhand descriptions.
During bedside report, nurses can:
- Confirm patient identity
- Visually assess the patient’s condition
- Check IV lines, pumps, drains, and monitors
- Identify safety risks such as fall precautions or pressure injury concerns
These real-time checks help reduce the chance of missing or inaccurate information. For example, an IV documented as running may actually be paused, infiltrated, or nearing completion. Verifying it at the bedside prevents delays and errors early in the shift.
Bedside shift report also helps identify discrepancies between documentation and reality. When both nurses observe the patient together, any questions can be addressed immediately rather than discovered hours later.
In this way, a bedside report provides an added layer of safety during one of the most error-prone moments in patient care: the transition between shifts.
Nurse Accountability and Error Prevention
Another significant benefit of bedside shift report is improved nurse accountability.
When the report occurs at the bedside, responsibility for patient care is clearly transferred. The incoming nurse starts the shift with a shared understanding of the patient’s status, priorities, and potential risks. The outgoing nurse confirms that critical information has been communicated and verified.
This shared process helps reduce:
- Ambiguity about patient condition
- Assumptions based on incomplete report
- Gaps in responsibility during shift change
Bedside shift report also discourages rushed or vague handoffs. Knowing the report will be reviewed at the bedside encourages more focused communication and reinforces professional standards.
From an error-prevention standpoint, this transparency matters. Clarifying details in real-time reduces reliance on memory and minimizes the likelihood of omissions that could affect care later in the shift.
Bedside Shift Report and Patient Satisfaction
While the bedside shift report is primarily focused on safety and communication, it also positively impacts how patients experience their care.
When patients are appropriately included in bedside report, they gain a clearer understanding of:
- Who is caring for them
- What the plan is for the upcoming shift
- What issues or goals are being monitored
This visibility can reduce confusion and build trust. Patients are less likely to feel that decisions are being made without their input or that important information is being discussed behind closed doors.
Importantly, patient involvement doesn’t mean disclosing every clinical detail at the bedside. Skilled nurses balance transparency with privacy by focusing on current care priorities and deferring sensitive discussions when needed.
When done effectively, a bedside shift report improves patient satisfaction by enhancing communication without compromising professionalism or confidentiality.
Is Bedside Shift Report Evidence-Based?
Bedside shift report is widely recognized as an evidence-based practice in nursing. However, it’s important to understand what this means in practical terms.
Evidence-based practice doesn’t imply that a single method works perfectly in every setting. Instead, it refers to care approaches that are supported by research, professional guidelines, and observed improvements in safety and quality when implemented correctly.
Research on bedside shift report consistently points to improvements in communication, a reduction in handoff errors, and stronger situational awareness during shift changes. These findings have prompted many healthcare organizations to adopt bedside reporting as part of broader patient safety and quality initiatives.
National patient safety efforts have also played a role. The Agency for Healthcare Research and Quality (AHRQ) has long emphasized the importance of structured handoffs and clear communication during transitions of care. Bedside shift report aligns with these recommendations by combining standardized communication with real-time verification at the bedside.
That said, the evidence shows an important limitation: bedside shift report is most effective when it is structured, consistent, and supported at the unit level. Units that implement bedside report without clear guidelines often report mixed results, including time pressure, incomplete information sharing, and staff frustration.
In short, the evidence supports the bedside shift report as a safety-focused practice—provided it’s applied thoughtfully, not mechanically.
Bedside Shift Report Checklist (What to Cover at the Bedside)
A bedside shift report checklist ensures that essential information is reviewed consistently during handoff. The checklist does not replace clinical judgment; its purpose is to reduce omissions during a high-risk transition.
Common items verified at the bedside include:
- Patient identification: Confirm the patient’s name and identifiers according to unit policy.
- Overall condition: Assess appearance, level of alertness, and comfort.
- Lines, drains, and airways: Verify IV sites, tubing, drains, oxygen delivery, and any devices in use.
- IV fluids, medications, and pumps: Check what’s running, remaining volumes, and pump settings.
- Pain and symptom management: Review current pain level, recent interventions, and response.
- Safety risks: Confirm fall risk status, mobility needs, alarms, and pressure injury precautions.
- Environment and equipment: Ensure the call light, bed position, and necessary supplies are in place.
- Patient questions or concerns: Allow time for brief clarification related to the current plan of care.
Sensitive, complex, or non-immediate information is typically addressed outside the room, either before or after the bedside portion of the report.
Bedside Shift Report Template (Simple, Realistic Format)
While the checklist focuses on what to verify, a bedside shift report template helps guide the flow of the report. A consistent structure improves clarity and keeps the handoff focused.
A practical bedside shift report template follows this sequence:
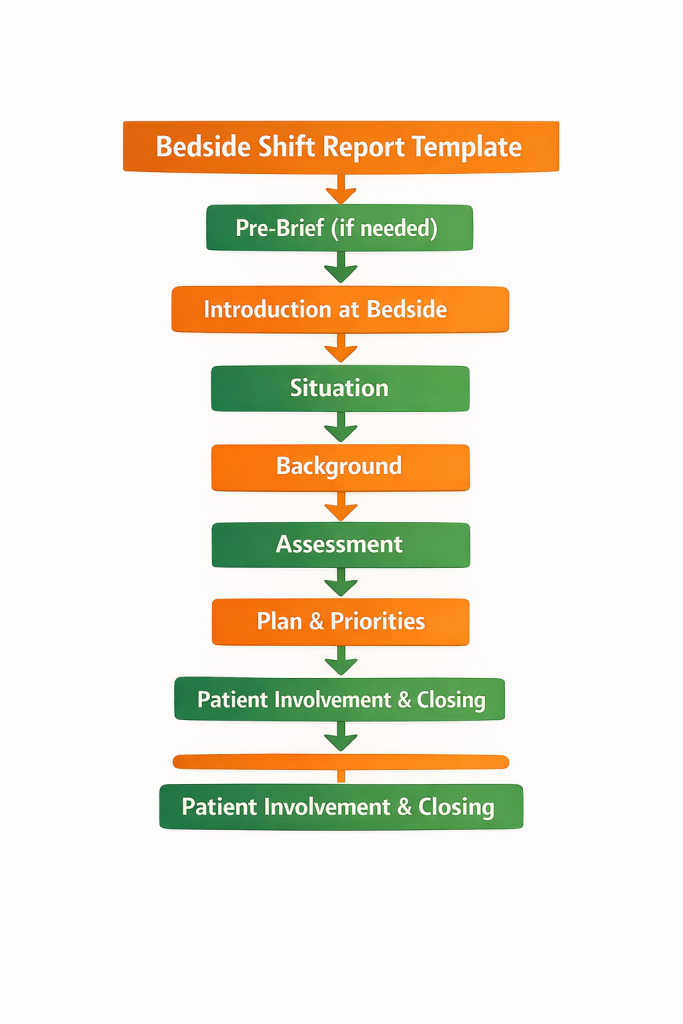
- Pre-brief (if needed): Discuss sensitive details or complex histories outside the room.
- Introduction at the bedside: Identify both nurses and explain the purpose of the handoff to the patient.
- Situation: State the patient’s primary diagnosis or reason for care and current status.
- Background: Share relevant background information that informs current care.
- Assessment: Review vital concerns, recent changes, safety risks, and key observations.
- Plan and priorities: Outline goals for the upcoming shift, pending tests, or anticipated needs.
- Patient involvement and closing: Invite patient questions and confirm the transfer of responsibility.
This structure keeps the report focused, efficient, and adaptable to different patient populations and care settings.
Bedside Shift Report Examples
Bedside shift report varies based on the patient’s condition, privacy needs, and unit workflow. Below are real-world examples demonstrating how bedside report might unfold in different scenarios. These examples focus on key observations and appropriate patient involvement.
Example 1: Standard Medical-Surgical Patient
- Step 1 – Introductions:
The outgoing nurse introduces the incoming nurse to the patient by name, ensuring both the patient and nurse are familiar with each other’s roles. The incoming nurse verifies the patient’s identity to prevent any errors. - Step 2 – Situation:
The outgoing nurse briefly outlines the patient’s reason for admission and current status. For example, “This patient is post-op from a hip replacement and is stable. Pain control and monitoring for signs of infection are key priorities.” - Step 3 – Joint Observation:
Both nurses conduct a joint assessment of the patient. They check the IV site, drains, oxygen levels, and any other equipment in use. The incoming nurse confirms that all necessary devices are functioning properly, while the outgoing nurse points out any key observations. “The IV is running at 100mL/hr, the patient’s pain score is 3/10, and all safety alarms are active.” - Step 4 – Plan Focus:
The outgoing nurse specifies key priorities for the shift. For example, “Continue monitoring pain levels every hour, and ensure the dressing is intact. The plan is to start physical therapy later today.” - Step 5 – Patient Questions:
After the exchange, the incoming nurse gives the patient a chance to ask any questions or voice concerns. For instance, “Is there anything you’d like to ask about your care today?” This ensures the patient is informed and involved in the care process.
Example 2: Higher-Acuity Patient with Complex Monitoring
- Pre-Bedside Discussion:
Before entering the room, the nurses review critical data that may not be suitable for bedside discussion, such as lab results or complex medication changes. This ensures privacy and prepares both nurses for a focused bedside exchange. - Step 1 – Bedside Portion:
Nurses enter the room and immediately verify the patient’s identity. The outgoing nurse explains key aspects of the patient’s condition. For example, “This patient is on a continuous morphine infusion for pain management and requires frequent respiratory monitoring.” - Step 2 – Joint Observation:
Both nurses verify the critical equipment in use, such as ventilators, IV pumps, and monitors. They ensure the patient’s airway is clear, confirm that all connections are intact, and check the overall patient environment. - Step 3 – Verification:
The incoming nurse repeats key points to confirm understanding. “So, we are continuing with the morphine drip, and respiratory therapy is scheduled for the next hour?” The outgoing nurse confirms, and they both check the patient’s respiratory rate and other vital signs. - Step 4 – Wrap-Up:
The patient is given an opportunity to ask any questions or voice concerns about the upcoming shift. “Do you have any questions about your care or what’s happening next?” This ensures that the patient is involved and has clarity about their care plan.
Example 3: Patient Sleeping or Unavailable
- Step 1 – Visual Scan:
If the patient is sleeping or temporarily unavailable, the nurses enter the room quietly and conduct a visual assessment of the patient’s condition and environment. The outgoing nurse points out key equipment such as the IV site, monitors, and alarms to the incoming nurse. - Step 2 – Minimal Verbal Report:
The outgoing nurse provides a brief summary of the patient’s current status without disturbing the patient. For example, “The patient is stable, with no new concerns. The IV is set to run at 50mL/hr, and there are no changes in respiratory status.” - Step 3 – Follow-Up Afterward:
Any additional details or sensitive information are discussed outside the room, ensuring that the patient’s rest is not interrupted. The incoming nurse is updated about the care plan, including any pending labs or treatments, without disturbing the patient.
Bedside Shift Report Examples
Bedside shift report varies based on the patient’s condition, privacy needs, and unit workflow. Below are real-world examples demonstrating how bedside report might unfold in different scenarios. These examples focus on key observations and appropriate patient involvement.
Example 1: Standard Medical-Surgical Patient
- Step 1 – Introductions:
The outgoing nurse introduces the incoming nurse to the patient by name, ensuring both the patient and nurse are familiar with each other’s roles. The incoming nurse verifies the patient’s identity to prevent any errors. - Step 2 – Situation:
The outgoing nurse briefly outlines the patient’s reason for admission and current status. For example, “This patient is post-op from a hip replacement and is stable. Pain control and monitoring for signs of infection are key priorities.” - Step 3 – Joint Observation:
Both nurses conduct a joint assessment of the patient. They check the IV site, drains, oxygen levels, and any other equipment in use. The incoming nurse confirms that all necessary devices are functioning properly, while the outgoing nurse points out any key observations. “The IV is running at 100mL/hr, the patient’s pain score is 3/10, and all safety alarms are active.” - Step 4 – Plan Focus:
The outgoing nurse specifies key priorities for the shift. For example, “Continue monitoring pain levels every hour, and ensure the dressing is intact. The plan is to start physical therapy later today.” - Step 5 – Patient Questions:
After the exchange, the incoming nurse gives the patient a chance to ask any questions or voice concerns. For instance, “Is there anything you’d like to ask about your care today?” This ensures the patient is informed and involved in the care process.
Example 2: Higher-Acuity Patient with Complex Monitoring
- Pre-Bedside Discussion:
Before entering the room, the nurses review critical data that may not be suitable for bedside discussion, such as lab results or complex medication changes. This ensures privacy and prepares both nurses for a focused bedside exchange. - Step 1 – Bedside Portion:
Nurses enter the room and immediately verify the patient’s identity. The outgoing nurse explains key aspects of the patient’s condition. For example, “This patient is on a continuous morphine infusion for pain management and requires frequent respiratory monitoring.” - Step 2 – Joint Observation:
Both nurses verify the critical equipment in use, such as ventilators, IV pumps, and monitors. They ensure the patient’s airway is clear, confirm that all connections are intact, and check the overall patient environment. - Step 3 – Verification:
The incoming nurse repeats key points to confirm understanding. “So, we are continuing with the morphine drip, and respiratory therapy is scheduled for the next hour?” The outgoing nurse confirms, and they both check the patient’s respiratory rate and other vital signs. - Step 4 – Wrap-Up:
The patient is given an opportunity to ask any questions or voice concerns about the upcoming shift. “Do you have any questions about your care or what’s happening next?” This ensures that the patient is involved and has clarity about their care plan.
Example 3: Patient Sleeping or Unavailable
- Step 1 – Visual Scan:
If the patient is sleeping or temporarily unavailable, the nurses enter the room quietly and conduct a visual assessment of the patient’s condition and environment. The outgoing nurse points out key equipment such as the IV site, monitors, and alarms to the incoming nurse. - Step 2 – Minimal Verbal Report:
The outgoing nurse provides a brief summary of the patient’s current status without disturbing the patient. For example, “The patient is stable, with no new concerns. The IV is set to run at 50mL/hr, and there are no changes in respiratory status.” - Step 3 – Follow-Up Afterward:
Any additional details or sensitive information are discussed outside the room, ensuring that the patient’s rest is not interrupted. The incoming nurse is updated about the care plan, including any pending labs or treatments, without disturbing the patient.
Disadvantages of Bedside Shift Report (and How Nurses Manage Them)
While the bedside shift report provides clear benefits, it also introduces challenges. Recognizing these limitations and addressing them thoughtfully helps maintain the practice’s effectiveness.
Privacy Concerns
Certain details are not appropriate to discuss at the bedside, such as sensitive diagnoses or private patient information. Nurses manage this by separating sensitive content from bedside verification. Critical information is reviewed outside the room before or after the bedside portion of the report.
Time Pressure
Bedside report can sometimes feel time-consuming, especially when there is a large patient load. To mitigate this, using clear templates and focused checklists can streamline the process, making it more efficient without sacrificing quality.
Interruptions
Patients or family members may interrupt the report with unrelated questions or requests. To handle this, nurses should set expectations at the start of the report, indicating that the patient will have an opportunity to ask questions at the end of the exchange.
Staff Resistance
Not all nurses are comfortable with bedside shift report, especially if they are accustomed to more traditional methods. Education, consistent practice, and leadership support can help nurses adapt to bedside reporting, ultimately improving its acceptance across the unit.
These challenges do not invalidate bedside shift report but highlight the need for thoughtful implementation. When these challenges are addressed, bedside report can become a valuable practice for improving communication and patient care.
How to Improve Bedside Shift Report on Your Unit
Improving bedside shift report starts with consistency and clarity. Key strategies include:
- Standardizing the process: Use a standard checklist and template across the unit to ensure that critical information is consistently covered.
- Defining boundaries: Clearly define what information belongs at the bedside and what should be discussed outside the room.
- Education and training: Provide ongoing education for nurses and staff, modeling best practices and offering feedback for improvement.
- Encouraging feedback: Solicit feedback from staff to identify areas for improvement and ensure that the process meets the needs of both patients and healthcare workers.
- Simple audits: Conduct audits to identify gaps in practice and ensure that the bedside shift report is consistently applied.
Units that treat bedside shift report as a shared professional practice, rather than just a task to complete, tend to see better outcomes and smoother handoffs. Ongoing evaluation and adaptation help make bedside shift report an integral and reliable part of nursing care.
Conclusion
Bedside shift report is a structured and effective method for transferring responsibility during one of the most critical transitions in nursing care. When applied thoughtfully, it strengthens communication, reinforces accountability, and enhances patient safety.
The success of bedside shift report hinges on balance: balancing structure with flexibility, patient involvement with privacy, and efficiency with thoroughness. While it is essential to have clear guidelines, it is equally important to adapt to the unique needs of each patient and unit.
By using checklists, templates, and real-world judgment, nurses can transform bedside shift report from a routine task into a powerful tool that improves the quality of patient care and enhances teamwork. As healthcare continues to prioritize patient safety and communication, bedside shift report will remain an invaluable practice in ensuring safer, more effective care transitions.
Ultimately, bedside shift report is not just about exchanging information—it’s about setting the stage for the next nurse to provide the best possible care, with the patient’s well-being at the heart of the handoff process.
Next Steps
To ensure continuous improvement:
- Keep adjusting the process as your unit’s needs evolve.
- Regularly evaluate the effectiveness of bedside shift report through feedback, audits, and staff input.
- Support training and education to ensure everyone is aligned with the standards.
By continuously refining bedside shift report, you create an environment where communication flows seamlessly, and patients feel heard and cared for during their most vulnerable moments.

