Giving end-of shift reports is one of the most important responsibilities in nursing. This is the moment when care is transferred from one nurse to another, and patient safety depends on how clearly that information is shared.
Many nurses find shift reports challenging, not because they lack knowledge, but because of the conditions in which the report takes place.
Common challenges during shift report
By the end of a shift:
- The unit is often busy and noisy.
- Time feels limited, especially during shift change.
- There is pressure not to forget important details.
- Fatigue can affect focus and memory.
When these factors come together, shift reports can feel rushed or overwhelming.
This guide is designed to reduce that stress by providing structure and clarity. You will learn:
- What an effective nursing end-of shift report includes
- How to organize your report using a simple, reliable structure
- How real nursing end-of shift report examples are put together
The goal is not to speak longer. The goal is to communicate clearly, accurately, and with purpose.
What Is a Nursing End-of Shift Report?
A nursing end-of shift report is a structured handoff in which one nurse transfers responsibility for patient care to the next nurse at the end of a shift.
Its purpose is to make sure care continues safely and smoothly.
What information an end-of shift report communicates
An effective end-of shift report answers four key questions for the oncoming nurse:
A. What is the patient’s current condition?
B. What happened during this shift?
C. What still needs to be done?
D. What should be monitored closely on the next shift?
When these questions are answered clearly, the next nurse can prioritize care without confusion or delay.
Why end-of shift report is Important
End-of shift report supports continuity of care. Without a clear handoff:
- Important details can be missed
- Tasks may be delayed or duplicated
- Early signs of patient decline may go unnoticed
This is why healthcare facilities emphasize clear handoff communication and standardized reporting practices.
What a Nursing End-of Shift Report Is Not
Understanding what does not belong in shift report is just as important as knowing what does.
An end-of shift report is not:
- A full review of the patient’s medical record
- A list of every lab result or medication
- A repetition of information that is easy to find in the chart
Instead, it focuses on key information that affects care right now.
The chart provides detailed documentation. Shift report provides clinical insight, priorities, and direction.
Why Nursing End-of Shift Report Is Critical
A well-given end-of shift report directly affects patient outcomes.
How clear shift report supports safe care
Clear and organized reports help to:
- Reduce medication and treatment errors
- Prevent missed tests or follow-up tasks
- Identify early signs of patient decline
- Improve teamwork and communication between nurses
In contrast, incomplete or unclear reports can lead to confusion, repeated work, or safety risks.
Using a structured approach protects both the patient and the nurse by reducing uncertainty and miscommunication.
Nursing End-of Shift Report Template (Simple SBAR Format)
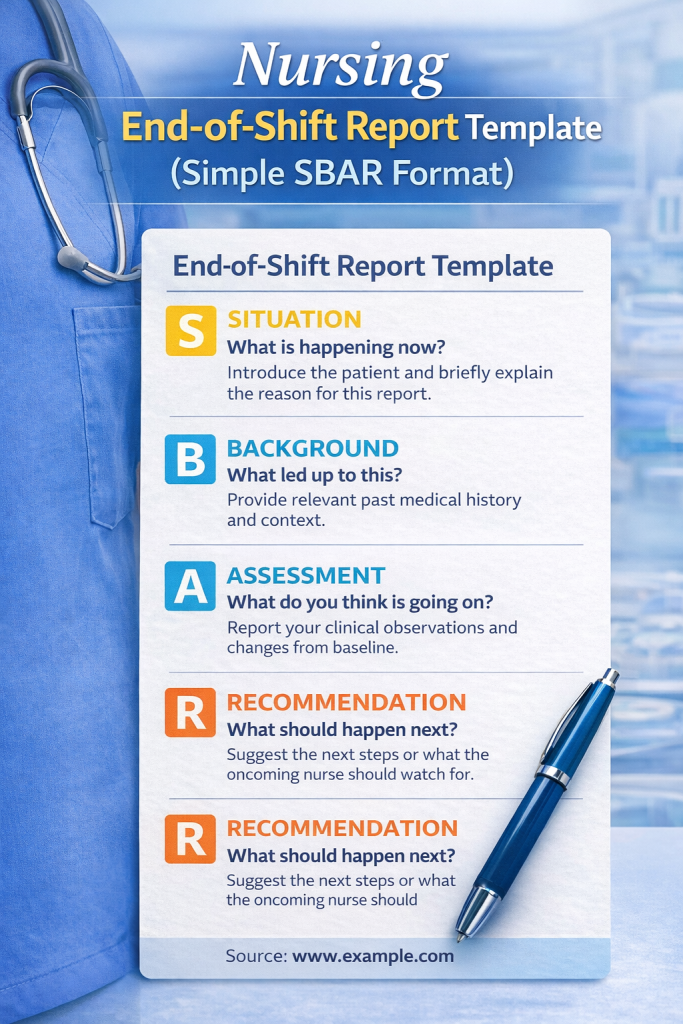
One of the most reliable ways to organize an end-of shift report is by using the SBAR format. SBAR gives your report a clear flow and helps ensure that important information is not missed, even when the unit is busy or you are tired.
SBAR stands for:
- Situation
- Background
- Assessment
- Recommendation
Each part serves a specific purpose in the handoff process.
S — Situation: Set the Clinical Picture
The Situation briefly explains who the patient is and what is happening right now. This is where you orient the oncoming nurse.
At a minimum, this section should answer:
- Who is the patient?
- Why are they here?
- How are they doing at this moment?
For example, instead of listing many details, you might say that the patient is stable, declining, or being closely monitored. This allows the next nurse to immediately understand the level of concern.
The situation should be short. Its job is to set the stage, not tell the whole story.
B — Background: Share Only What Matters
The Background provides context that helps explain the patient’s current condition.
This may include:
- The reason for admission
- Relevant medical history
- Information from previous shifts that affects care
Not all history belongs here. Focus only on details that help the next nurse understand why the patient is in their current state.
For example, long-standing conditions may be mentioned briefly, while recent surgeries or complications deserve more attention.
A — Assessment: Explain What You Observed
The Assessment is where your nursing judgment becomes important.
This section focuses on:
- What you observed during your shift
- Changes from baseline
- Abnormal findings or trends
Rather than listing normal values, explain what stood out. For instance, trends in vital signs or changes in behavior are often more important than single measurements.
If nothing changed during your shift, it is appropriate to say that clearly. Stability is still meaningful information.
R — Recommendation: Guide the Next Shift
The Recommendation tells the oncoming nurse what needs to happen next.
This may include:
- Tasks that still need to be completed
- Medications, labs, or treatments due
- Concerns that require close monitoring
This part of the report helps prioritize care. Clear recommendations reduce confusion and prevent missed or delayed actions.
If there is something you are concerned about, this is where you should state it directly.
Nursing End-of Shift Report Examples
The following examples show how an end-of shift report can be organized using the SBAR structure. They are meant to demonstrate how information is prioritized and communicated, not to serve as scripts.
Each example focuses on what the oncoming nurse needs to know to continue care safely and efficiently.
End-of Shift Report Example 1: Med-Surg Patient With Stable Condition
Situation
The patient is a 62-year-old admitted for community-acquired pneumonia. They are currently stable on room air and have had no acute issues during this shift.
Background
The patient was admitted two days ago with shortness of breath and fever. They are being treated with IV antibiotics and have no significant cardiac history. Code status is full code, and there are no known drug allergies.
Assessment
During this shift, the patient remained hemodynamically stable. Oxygen saturation stayed within baseline on room air, and lung sounds were unchanged. The patient tolerated meals well and was able to ambulate to the bathroom with minimal assistance. No new complaints were reported, and pain was denied.
Recommendation
Continue current antibiotic therapy as ordered. Monitor respiratory status and temperature trends. Encourage use of the incentive spirometer and ambulation as tolerated. Morning labs are scheduled and should be reviewed when available.
End-of Shift Report Examples 2: Post-Operative Patient (First 24 Hours)
Situation
The patient is a 48-year-old who is post-operative day one following a laparoscopic cholecystectomy. The patient is alert, hemodynamically stable, and recovering on the medical-surgical unit.
Background
The patient was admitted for elective surgery and has no significant past medical history. The procedure was completed without complications. Code status is full code, and there are no known drug allergies.
Assessment
During this shift, the patient’s vital signs remained stable. Pain was reported at a moderate level and was managed with prescribed analgesics, with good relief noted. The surgical incisions are clean, dry, and intact with no signs of infection. The patient tolerated clear liquids and ambulated in the hallway with standby assistance. Urine output was adequate, and bowel sounds were present.
Recommendation
Continue to monitor pain levels and administer analgesics as ordered. Encourage continued ambulation and use of the incentive spirometer. Advance diet as tolerated per post-operative orders. Monitor incision sites for signs of infection and reinforce post-operative teaching as needed.
End-of Shift Report Examples 3: Deteriorating Patient With Change in Condition
Situation
The patient is a 70-year-old admitted for a urinary tract infection who has shown a change in condition during this shift. The patient is currently febrile and more lethargic than earlier in the day.
Background
The patient was admitted yesterday with confusion and dysuria. Past medical history includes hypertension and type 2 diabetes. The patient is receiving IV antibiotics. Code status is full code, with no known drug allergies.
Assessment
During this shift, the patient developed an elevated temperature and increasing confusion. Vital signs showed a rising heart rate and lower blood pressure compared to baseline. Urine output decreased, and the patient required increased assistance with mobility. The provider was notified, blood cultures were drawn, and IV fluids were started per new orders.
Recommendation
Continue close monitoring of vital signs and mental status. Maintain IV fluids as ordered and monitor urine output closely. Follow up on blood culture results when available. Notify the provider of any further decline or lack of response to treatment.
End-of Shift Report Examples 4: Telemetry Patient With Respiratory Support
Situation
The patient is a 65-year-old admitted for acute exacerbation of chronic obstructive pulmonary disease. The patient is currently on telemetry and receiving supplemental oxygen via nasal cannula.
Background
The patient was admitted two days ago with shortness of breath and wheezing. Past medical history includes COPD and a history of smoking. The patient is receiving bronchodilator treatments and steroids. Code status is full code.
Assessment
During this shift, the patient remained stable on two liters of oxygen with oxygen saturation within baseline range. Breath sounds remained diminished bilaterally with intermittent wheezing. The patient required scheduled breathing treatments, which improved work of breathing. No chest pain or cardiac rhythm changes were noted on telemetry.
Recommendation
Continue oxygen therapy and respiratory treatments as ordered. Monitor oxygen saturation and respiratory effort, especially with activity. Encourage use of pursed-lip breathing and allow rest periods. Report any increase in oxygen needs or respiratory distress.
End-of Shift Report Examples 5: Heart Failure Patient With Fluid Balance Concerns
Situation
The patient is a 72-year-old admitted for acute decompensated heart failure. The patient is currently stable but requires close monitoring of fluid status.
Background
The patient was admitted three days ago with shortness of breath and lower extremity edema. Past medical history includes heart failure with reduced ejection fraction and hypertension. The patient is receiving diuretic therapy. Code status is full code.
Assessment
During this shift, the patient remained hemodynamically stable. Lung sounds were diminished at the bases with mild crackles noted. Intake and output were closely monitored, with a net negative balance by the end of the shift. The patient reported improved breathing compared to the previous day but continued to have mild lower extremity edema.
Recommendation
Continue diuretic therapy as ordered and monitor intake and output closely. Obtain daily weights as scheduled and compare to baseline. Monitor respiratory status and notify the provider of any increase in shortness of breath or weight gain.
End-of Shift Report Examples 6: Diabetic Patient With Blood Glucose Variability
Situation
The patient is a 55-year-old admitted for management of uncontrolled type 2 diabetes. The patient is currently stable but has experienced fluctuating blood glucose levels.
Background
The patient was admitted for hyperglycemia and medication adjustment. Past medical history includes type 2 diabetes and obesity. The patient is receiving scheduled insulin with sliding scale coverage. Code status is full code.
Assessment
During this shift, blood glucose levels fluctuated despite insulin administration. One episode of hypoglycemia occurred and was treated per protocol, with good response. The patient tolerated meals and denied symptoms of dizziness or weakness after treatment. No other acute issues were noted.
Recommendation
Continue scheduled glucose monitoring and insulin coverage as ordered. Monitor closely for signs of hypoglycemia, especially around meals. Reinforce diabetes education as appropriate and communicate any further glucose instability to the provider.
What to Include in a Nursing End-of Shift Report
One of the hardest parts of a shift report is deciding what is important enough to say out loud. A good end-of shift report is selective. It does not include everything you know about the patient. It includes what the next nurse needs to know to provide safe care.
A helpful way to think about this is to focus on information that affects the next shift.
1. Patient Identification and Overall Status
Every report should begin by clearly identifying the patient and their general condition. This helps the oncoming nurse quickly orient themselves.
At this point, you should establish:
- Who the patient is
- Why they are admitted
- How they are doing overall
Stating whether the patient is stable, improving, or declining gives immediate clinical context and helps the next nurse set priorities.
2. Code Status and Allergies
Code status and allergies should always be communicated clearly, even if they are documented elsewhere.
These details affect urgent decision-making. During emergencies, nurses do not have time to search the chart. Hearing this information during report ensures it is fresh and understood.
If there are no known allergies or the code status is unchanged, it is still appropriate to state that briefly.
3. Vital Signs and Clinical Trends
Rather than listing numbers, focus on patterns and changes.
For example:
- Are vital signs stable or trending in a concerning direction?
- Did the patient require intervention for abnormal values?
- Was monitoring increased during your shift?
Explaining trends helps the next nurse anticipate potential issues, which is more useful than isolated readings.
4. Lines, Drains, Airways, and Oxygen
Any device attached to the patient should be included in report because it requires monitoring and care.
This includes:
- IV access and fluids
- Central lines, Foley catheters, or drains
- Oxygen devices and flow rates
It is especially important to mention problems, such as difficulty maintaining IV access, leaking drains, or increased oxygen needs. These details directly affect the next shift’s workload.
5. Pain and Comfort
Pain management is a key part of nursing care and should not be overlooked during report.
You should communicate:
- Where the patient is experiencing pain
- How severe it is
- Whether interventions were effective
If pain is not well controlled, that information helps the next nurse plan reassessment and intervention early in the shift.
6. Mobility, Safety, and Skin Integrity
Safety-related information helps prevent falls and injuries.
This section may include:
- Level of mobility or assistance required
- Fall risk status
- Skin concerns or wounds
Even small changes, such as increased weakness or new redness, are worth mentioning because they may signal developing problems.
7. Medications and Treatments Requiring Follow-Up
Routine medications do not need to be reviewed in detail unless there is an issue.
Focus instead on:
- Time-sensitive medications
- Medications that were held or refused
- Treatments that are still pending
This helps the next nurse avoid delays or missed care.
8. Labs, Tests, and Consults
This part of the report prepares the next nurse for what is coming.
Important details include:
- Abnormal labs that need follow-up
- Tests ordered but not yet completed
- Consults that are expected or already involved
Mentioning what is pending prevents surprises during the next shift.
9. Discharge Planning (When Relevant)
If discharge is expected soon, it should be mentioned briefly.
This may include:
- Expected discharge timing
- Barriers to discharge
- Education that has been completed or still needed
Discharge planning often begins before the day of discharge, so early communication is helpful.
How to Give an Effective Nursing End-of Shift Report
What you say during a report is important, but how you deliver it often determines whether the information is understood and used correctly. An effective end-of shift report is organized, focused, and easy to follow.
This section explains practical habits that improve report quality without making it longer.
Use the Same Structure for Every Patient
Consistency is one of the strongest tools in safe communication.
When you give report in the same order for every patient:
- The oncoming nurse knows what to expect
- Information is easier to process
- Important details are less likely to be missed
Using a structured format, such as SBAR, helps keep your report predictable and organized, especially when you are handing off care for multiple patients.
Start With the Big Picture, Then Add Detail
Effective reports move from general to specific.
Begin with:
- Who the patient is
- Why they are admitted
- Their overall condition
Once the listener understands the situation, additional details make more sense. Jumping straight into lab values or tasks without context can cause confusion.
Focus on What Changed During Your Shift
The most valuable part of end-of shift report is new or changing information.
This may include:
- New symptoms
- Worsening or improving conditions
- Unexpected events
- Changes in treatment or response
The next nurse can review the chart for background information. Your role during report is to highlight what is different or concerning.
If nothing changed, it is appropriate to say so clearly. Stability is important information.
Avoid Reading the Chart Word for Word
Shift report is not a chart review.
Reading directly from the chart:
- Slows down report
- Makes it harder to identify priorities
- Reduces meaningful communication
Instead, summarize the information and explain its significance. This shows clinical understanding and helps the next nurse apply the information to patient care.
Be Clear About Priorities and Expectations
A strong end-of shift report helps the next nurse plan their time.
When possible, clarify:
- What needs to be done first
- What requires close monitoring
- What could become a problem later in the shift
Clear recommendations reduce uncertainty and prevent missed tasks.
Keep the Report Professional and Objective
End-of shift report should remain factual and focused.
Avoid:
- Personal opinions
- Assumptions
- Emotional language
Professional, objective language supports safe communication and mutual respect among team members.
Allow Time for Questions and Clarification
End-of shift report is a shared responsibility.
After giving report:
- Pause briefly
- Invite questions
- Clarify any unclear points
This step helps confirm understanding and reduces the chance of errors.
End-of Shift Report vs. Bedside Shift Report: What’s the Difference?
End-of shift report and bedside shift report are often discussed together, which can make them seem interchangeable. In practice, they serve related but distinct roles in nursing communication.
Understanding the difference helps nurses choose the right approach while maintaining patient safety and professionalism.
End-of Shift Report: The Core Handoff
An end-of shift report is the formal transfer of responsibility for patient care from one nurse to another at the end of a shift.
Its primary purpose is communication. The off-going nurse ensures the oncoming nurse understands:
- The patient’s current condition
- What occurred during the shift
- What still needs to be done
- What requires close monitoring
The defining feature of end-of shift report is what information is communicated, not where the report takes place.
End-of shift report may occur:
- At the nurses’ station
- In a report room
- In a hallway
- At the bedside
Regardless of location, this handoff must occur every shift.
Bedside Shift Report: A Specific Method
A bedside shift report is one method of delivering an end-of shift report. It takes place in the patient’s room and includes the patient in the process.
In addition to sharing information, bedside shift report often involves:
- Visual assessment of the patient
- Equipment and safety checks
- Limited patient participation
Bedside shift report adds a location and interaction component, but it does not change the core purpose of the handoff.
How the Two Are Related
The relationship between the two can be summarized simply:
End-of shift report is required.
Bedside shift report is optional and situational.
All bedside shift reports are end-of shift reports, but not all end-of shift reports are done at the bedside.
Many facilities encourage a hybrid approach, where:
- Safety-focused information is shared at the bedside
- Sensitive or complex details are discussed privately
This allows nurses to balance transparency, efficiency, and patient privacy.
Knowing the difference allows nurses to communicate more effectively while maintaining professional boundaries.
Conclusion: Making End-of Shift Report Clear, Consistent, and Safe
Nursing end-of shift report plays a central role in safe patient care. It is the point where responsibility transfers, and clear communication determines how smoothly care continues into the next shift.
A strong report is not about sharing more information. It is about sharing the right information in a clear and organized way. Using a structured approach such as SBAR helps nurses focus on patient priorities, highlight changes, and communicate expectations for the next shift.
Understanding what to include, what to leave out, and how to deliver report makes the process more efficient and less stressful. It also reduces the risk of miscommunication, missed tasks, and delays in care.
It is equally important to recognize the difference between end-of shift report and bedside shift report. End-of shift report is the required handoff of responsibility, while bedside shift report is one method of delivering that handoff when appropriate.
The nursing end-of shift report examples that follow show how these principles are applied in real clinical situations. By focusing on structure, clarity, and relevance, nurses can give reports that support continuity of care and patient safety at every shift change.
Frequently Asked Questions About Nursing End-of Shift Report
- How long should a nursing end-of shift report be?
A nursing end-of shift report should be brief but complete. For most patients, a clear report takes about one to three minutes.
The exact length depends on:
- How complex the patient’s condition is
- Whether anything changed during the shift
- What tasks or concerns carry over to the next shift
A longer report does not mean a better report. What matters most is that the oncoming nurse understands the patient’s current status and priorities.
- Do I need to use SBAR for end-of shift report?
SBAR is not required in every facility, but it is widely recommended because it improves clarity and consistency.
Using SBAR helps nurses:
- Organize information logically
- Reduce missed or forgotten details
- Communicate more clearly across experience levels
Even if your unit does not formally require SBAR, using it can make your reports easier to follow and more effective.
- What is the most important part of an end-of shift report?
The most important part of end-of shift report is what changed during your shift.
This includes:
- New symptoms
- Changes in vital signs or condition
- Worsening or improvement
- New orders, treatments, or concerns
If nothing changed, stating that clearly is still important. Stability helps the next nurse plan care with confidence.
- Should I include normal findings in my report?
Normal findings usually do not need to be included unless they add meaning.
You should mention normal findings when:
- They represent a change from baseline
- They help explain a concern
- They are critical to ongoing monitoring
For example, stable vital signs may not need discussion, but stable oxygen levels in a respiratory patient may still be relevant
- What if I forget something after I give report?
If you remember important information after report:
- Notify the oncoming nurse as soon as possible
- Clarify the detail directly
- Document appropriately if required
Clear follow-up communication is always better than assuming the detail is unimportant.
- Can nursing students use templates for end-of shift report?
Yes. Templates are especially helpful for nursing students and new graduate nurses.
Templates:
- Provide structure
- Reduce anxiety during report
- Help build confidence
With experience, most nurses naturally adapt templates to fit their workflow and unit expectations.
- Is end-of shift report a legal requirement?
While specific rules vary by facility, end-of shift report is considered a professional responsibility in nursing.
Clear handoff communication:
- Supports patient safety
- Demonstrates accountability
- Reduces risk related to miscommunication
Incomplete or unclear reports increase the likelihood of errors and may place both patients and nurses at risk.

