In nursing, communication is more than just exchanging information. It’s about building trust, showing empathy, and supporting patients throughout their healthcare journey. Therapeutic communication plays a crucial role in fostering these connections and improving patient outcomes.
In this article, we will explore how therapeutic communication nursing scenarios examples can enhance your practice as a nurse. We’ll discuss key techniques nurses use to engage with patients effectively, why these methods are essential in patient care, and provide practical scenarios that demonstrate how these techniques are applied in real-world nursing situations.
What is Therapeutic Communication in Nursing?
Therapeutic communication in nursing refers to the use of verbal and non-verbal communication techniques to promote healing and understanding between nurses and patients. Unlike casual conversation, therapeutic communication is intentional and goal-oriented. It aims to create a supportive environment where patients feel heard and understood.
This type of communication is vital for building trust. When nurses use therapeutic communication, patients are more likely to open up about their concerns, symptoms, and emotional state. This openness leads to better care and more accurate assessments of the patient’s needs.
In essence, therapeutic communication is not just about talking; it’s about creating a connection that helps improve the patient’s overall well-being and experience.
Therapeutic Communication Techniques in Nursing
Therapeutic communication techniques are specific strategies that nurses use to establish a supportive and understanding relationship with their patients. These techniques help to clarify, encourage openness, and foster trust. Here are some of the most commonly used techniques in nursing practice:
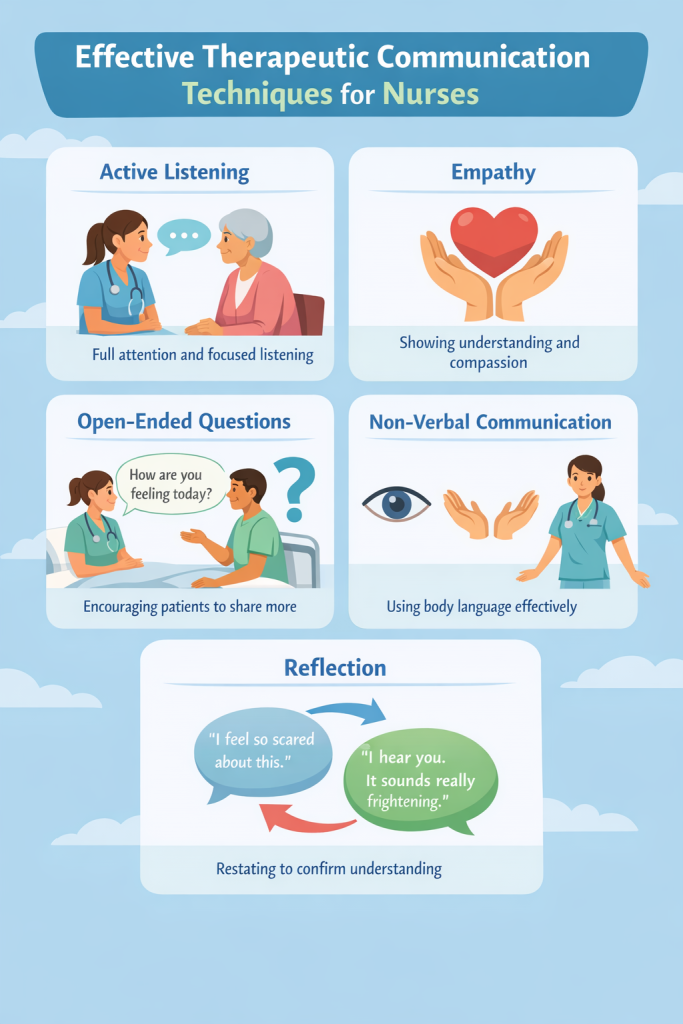
- Active Listening: This is perhaps the most crucial skill. It involves fully focusing on the patient, not interrupting, and reflecting on what they are saying to show understanding.
- Empathy: Empathy is about acknowledging the patient’s emotions without judgment. It helps to communicate that the nurse cares about the patient’s well-being and is there to support them.
- Open-Ended Questions: By asking questions that can’t be answered with a simple “yes” or “no,” nurses encourage patients to elaborate on their feelings and experiences. This promotes deeper conversation and understanding.
- Reflection: Paraphrasing or repeating what the patient says to confirm understanding. This assures patients that they are being heard and their concerns are valid.
- Non-Verbal Cues: Body language, eye contact, and facial expressions all contribute to the communication process. Non-verbal cues can express care and understanding even without words.
These techniques help nurses build rapport and engage patients in a way that fosters healing and trust.
Therapeutic Communication Nursing Scenarios Examples
In nursing, applying therapeutic communication techniques can be challenging, especially in emotionally charged situations. Using the right communication methods in real-life scenarios can make a significant difference in how patients feel about their care.
Therapeutic communication is especially important when nurses face emotionally intense moments with patients. Whether managing patient anxiety, offering emotional support, or addressing pain management, nurses use a variety of strategies to ensure the patient feels heard and supported.
Each interaction, no matter how small, is an opportunity to practice therapeutic communication. Understanding when and how to use these techniques in real situations is key to improving the patient experience and clinical outcomes.
Scenario 1: Managing Patient Anxiety Before Surgery
Situation:
A patient scheduled for surgery appears visibly anxious while sitting in the preoperative area. They are fidgeting, avoiding eye contact, and repeatedly asking about the procedure, showing clear signs of worry. The nurse notices these signs of distress and approaches the patient with the intention of addressing their anxiety.
Therapeutic Communication Techniques Used:
- Active Listening: The nurse begins by sitting down next to the patient and gently says, “I can see you’re feeling a bit anxious about the surgery. Can you tell me what’s on your mind?” This open-ended question invites the patient to express their concerns. The nurse listens attentively, nodding and maintaining eye contact to show they are fully present in the conversation.
- Empathy: Recognizing the patient’s fear, the nurse responds with empathy: “I understand how you’re feeling. It’s completely normal to feel nervous before surgery, and I’m here to help you through this.” This acknowledges the patient’s emotions without judgment.
- Reassurance and Clarification: To further ease the patient’s mind, the nurse explains the surgical process step by step: “Let me walk you through what will happen today. You’ll be taken to the operating room, and the anesthesia team will make sure you’re comfortable and pain-free. We’ll be with you the whole time to make sure everything goes smoothly.” The nurse encourages the patient to ask any additional questions, ensuring they have a clear understanding of the process.
Outcome:
By using active listening to engage the patient and empathy to validate their feelings, the nurse helps the patient feel heard and understood. The nurse’s clear explanation of the surgical procedure provides much-needed clarity, reducing the patient’s anxiety. As a result, the patient feels more relaxed and better prepared, increasing their confidence in the care team and improving the overall experience.
Scenario 2: Supporting a Terminally Ill Patient
Situation:
A terminally ill patient in a hospice care setting expresses fear and uncertainty about their prognosis. They are visibly upset and reluctant to discuss their feelings with the healthcare team. The nurse notices the patient’s distress and decides to open a supportive dialogue.
Therapeutic Communication Techniques Used:
- Active Listening: The nurse begins by sitting down next to the patient, giving them space to express themselves. “I can see this is a tough time for you,” the nurse says softly. “I’m here to listen if you want to talk about what’s on your mind.” The nurse waits patiently, allowing the patient to speak without rushing them.
- Reflection: The patient mentions, “I’m scared of what’s coming, and I don’t know how to face it.” The nurse reflects the patient’s feelings to ensure they feel understood, saying, “It sounds like you’re really scared about what lies ahead. I can imagine that must be incredibly difficult to face.” This encourages the patient to explore their emotions further.
- Open-Ended Question: The nurse gently prompts the patient to share more, asking, “What are some of your concerns that we haven’t talked about yet?” This question opens the door for the patient to express their fears or ask any lingering questions about their care.
- Empathy and Reassurance: The nurse offers empathy and emotional support: “I’m here with you through this, and I want to make sure you feel comfortable with every step of your care. It’s okay to feel scared, and you don’t have to go through this alone.”
Outcome:
Through active listening and empathy, the nurse creates a safe space for the patient to share their fears and concerns. The nurse’s response helps the patient feel heard and understood, which in turn promotes emotional relief. The patient feels more comfortable discussing their condition, which leads to improved mental and emotional well-being, reducing feelings of isolation and fear.
Scenario 3: Addressing Pain Management Concerns Post-Surgery
Situation:
A patient recovering from surgery is in significant pain but hesitates to speak up about it. They avoid eye contact and seem uncomfortable when the nurse checks in. The nurse notices the patient’s tense posture and decides to address the situation.
Therapeutic Communication Techniques Used:
- Non-Verbal Cues: The nurse observes the patient’s facial expression and body language, noticing signs of discomfort, such as tightness in the chest and shallow breathing. The nurse gently asks, “I see you’re holding your abdomen—how would you rate your pain on a scale of 1 to 10?” This approach helps the patient feel more comfortable discussing their pain without feeling pressured.
- Clarification: The patient responds, “It hurts a lot, but I don’t want to bother anyone.” The nurse reassures them, “It’s never a bother to speak up about your pain. Pain management is a big part of your recovery, and we want to make sure you’re as comfortable as possible.” This clarification helps the patient understand that their comfort is a priority.
- Open-Ended Question: The nurse encourages the patient to describe their pain more specifically by asking, “Can you tell me where the pain is the most intense and if there’s anything that makes it better or worse?” This question gives the patient the opportunity to explain their experience in more detail.
- Empathy: Recognizing the patient’s hesitation, the nurse empathizes: “I understand that you may not want to take more medication, but we can work together to find the right solution for your comfort. Let’s make sure we’re managing this pain properly.”
Outcome:
By using non-verbal cues and clarification, the nurse helps the patient feel more comfortable discussing their pain. The open-ended question allows the nurse to better understand the specifics of the pain, leading to more effective pain management. As a result, the patient feels heard and supported, and their pain is better managed, promoting a quicker and more comfortable recovery.
Why is Therapeutic Communication Important in Nursing?
Therapeutic communication is one of the cornerstones of effective nursing practice. It is essential because it directly influences patient outcomes, satisfaction, and the overall quality of care. Nurses who practice therapeutic communication can provide emotional support, ensure patient comfort, and enhance the overall patient experience.
Here are the key reasons why therapeutic communication is so important in nursing:
- Builds Trust
When nurses use therapeutic communication, they establish trust with their patients. This trust is crucial for patients to feel comfortable sharing personal and sensitive health information. Trust also enables patients to feel confident in their care, which can lead to better adherence to treatment plans and recommendations. - Reduces Anxiety and Stress
Communication that acknowledges the patient’s feelings and concerns can significantly reduce anxiety. For example, a calm and empathetic conversation can help alleviate a patient’s fears before a procedure. By addressing the emotional aspects of care, nurses help patients manage their stress, which has been shown to improve recovery outcomes. - Improves Patient Satisfaction
Effective communication makes patients feel respected, valued, and heard. This leads to a higher level of satisfaction with the care they receive. When patients feel their concerns are taken seriously, they are more likely to trust the healthcare system and return for future care if needed. - Facilitates Accurate Information Exchange
Clear communication helps nurses gather accurate information from patients, such as symptoms, feelings, and medical history. This is critical for making informed clinical decisions. Miscommunication can lead to errors in diagnosis or treatment, so it’s vital that nurses use therapeutic communication to ensure that all information is understood correctly. - Enhances Patient Compliance
Patients who feel engaged in their care are more likely to follow the nurse’s advice and adhere to treatment protocols. Therapeutic communication enables nurses to explain treatment plans and medications clearly, helping patients understand the benefits and importance of their care. As a result, patients are more likely to be compliant, which can improve overall health outcomes. - Supports Holistic Care
Nurses who practice therapeutic communication are not only addressing the patient’s physical needs but also their emotional and psychological well-being. By establishing a rapport with the patient, nurses are able to assess and address issues like anxiety, fear, or depression that may affect the patient’s overall health and recovery. - Prevents and Reduces Medical Errors
Effective communication is key to preventing misunderstandings and mistakes in patient care. Miscommunication among healthcare teams, or between the nurse and patient, can lead to medication errors, incorrect procedures, or delays in care. Therapeutic communication ensures that information is shared clearly and accurately, reducing the risk of these errors. - Promotes Better Health Outcomes
Research has shown that patients who experience positive, empathetic communication from their healthcare providers are more likely to have better health outcomes. This is particularly true for patients dealing with chronic conditions or serious illnesses, where mental and emotional well-being plays a significant role in recovery.
By prioritizing therapeutic communication, nurses can enhance the care experience, address patients’ emotional and psychological needs, and ultimately improve patient outcomes.
Non-Therapeutic Communication in Nursing
While therapeutic communication fosters trust and improves patient care, non-therapeutic communication can have the opposite effect. Non-therapeutic communication refers to any verbal or non-verbal behavior that blocks effective communication or undermines the nurse-patient relationship. This can lead to frustration, mistrust, and misunderstandings.
Here are some common non-therapeutic communication behaviors to avoid:
- Offering False Reassurance: Telling a patient “Don’t worry, everything will be fine” when the situation may not warrant such assurance can lead to feelings of dismissal or invalidation.
- Changing the Subject Abruptly: If a patient is sharing their concerns or fears, abruptly changing the topic can make the patient feel unheard or neglected.
- Providing Unsolicited Advice: Offering advice without fully understanding the patient’s needs or perspective can feel like judgment rather than support.
- Giving Cliché Responses: Responses like “Everything happens for a reason” can seem dismissive of the patient’s emotional state and fail to acknowledge their individual experience.
- Judgmental or Moralizing Statements: Statements like “You shouldn’t feel that way” or “You need to do this for your health” can create a barrier, making patients feel unsupported or misunderstood.
Non-therapeutic communication does not only impact the nurse-patient relationship but can also lead to poor patient outcomes. Patients may feel reluctant to express their concerns or may withdraw emotionally, which can hinder proper care and treatment.
How to Improve Therapeutic Communication in Nursing
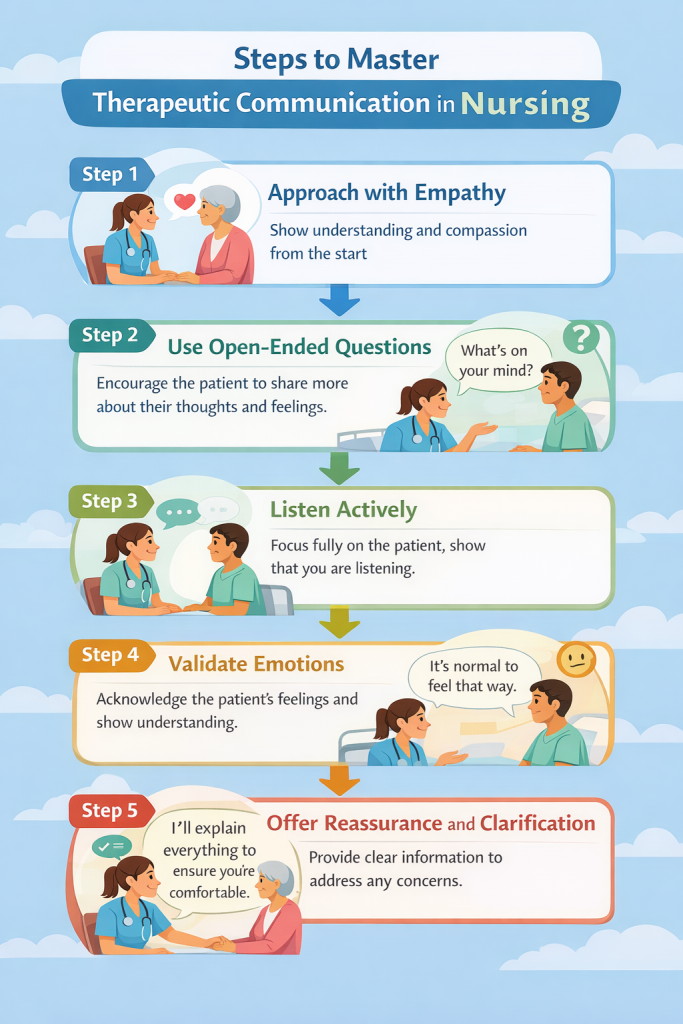
Improving therapeutic communication requires intentional effort and practice. Nurses can develop stronger communication skills through training, self-reflection, and applying techniques in everyday patient interactions. Here are some practical steps nurses can take to enhance their therapeutic communication skills:
- Practice Active Listening
Always give the patient your full attention. Active listening is the foundation of good communication. Avoid distractions and focus on what the patient is saying. This helps you understand their needs and concerns more effectively. - Use Open-Ended Questions
Ask questions that encourage the patient to express their thoughts and feelings in detail. For example, instead of asking, “Are you feeling okay?” ask, “How are you feeling today?” This opens the door for the patient to elaborate and share more. - Show Empathy
Empathy is key to building trust and rapport. Acknowledge the patient’s feelings by saying, “I can understand why you might feel that way” or “It must be difficult to go through this.” Being empathetic shows that you care about the patient’s emotional well-being. - Improve Non-Verbal Communication
Pay attention to your body language, facial expressions, and tone of voice. Positive non-verbal cues, like maintaining eye contact and nodding, can help reinforce what you’re saying verbally. Non-verbal communication often speaks louder than words. - Be Clear and Concise
Use simple, clear language when explaining medical terms or procedures. Avoid jargon and make sure the patient understands what you’re saying. Rephrase complex information if necessary to ensure clarity. - Reflect and Summarize
After the patient has shared their thoughts, reflect on what they’ve said by summarizing key points. This not only shows you’re actively listening but also ensures that you fully understand the patient’s concerns. - Seek Feedback
Regularly seek feedback from patients on how they feel about the communication process. Do they feel heard? Are there any misunderstandings that need clarification? This feedback is vital for continuous improvement. - Engage in Communication Training
Nurses should participate in communication skills workshops and training. This helps them stay up to date with best practices and learn new strategies to improve their communication with patients.
By improving therapeutic communication, nurses can build stronger, more positive relationships with their patients. This, in turn, leads to better care and improved patient outcomes.
Conclusion
Therapeutic communication is a fundamental skill for nurses that significantly impacts patient care. By practicing effective communication techniques, nurses can build trust, reduce anxiety, and improve patient satisfaction and outcomes. Whether it’s through active listening, showing empathy, or using open-ended questions, each interaction provides an opportunity to connect with the patient on a deeper level.
Effective communication goes beyond words; it involves body language, tone of voice, and attentiveness, all of which contribute to a holistic care experience. Nurses who prioritize therapeutic communication can foster a more supportive and healing environment for their patients, ensuring that care is not only physically effective but emotionally and psychologically beneficial as well.
As nursing practice continues to evolve, therapeutic communication remains a cornerstone of providing high-quality, patient-centered care. Nurses must continuously refine these skills through practice, training, and self-reflection to enhance both their professional development and the patient experience.

