Ever noticed a few colleagues with titles like RN II or RN III on their badges and wondered what those extra letters mean? That’s the nursing clinical ladder at work — a structured program that rewards growth, skill, and dedication beyond just years on the job.
Instead of feeling stuck in the same position, a clinical advancement program gives you measurable milestones, opportunities for recognition, and even pay incentives for the expertise you build over time.
In this guide, you’ll explore real nursing clinical ladder examples from hospitals, and discover practical tips to help you move confidently through each level. Whether you’re a new grad setting your sights on RN II or a nurse manager improving your team’s ladder, this article will show you exactly how these programs work — and how they can elevate your career.
What Is a Nursing Clinical Ladder?
A nursing clinical ladder (sometimes called a clinical advancement program) is a clear, step-by-step framework that recognizes and rewards nurses for professional growth and excellence.
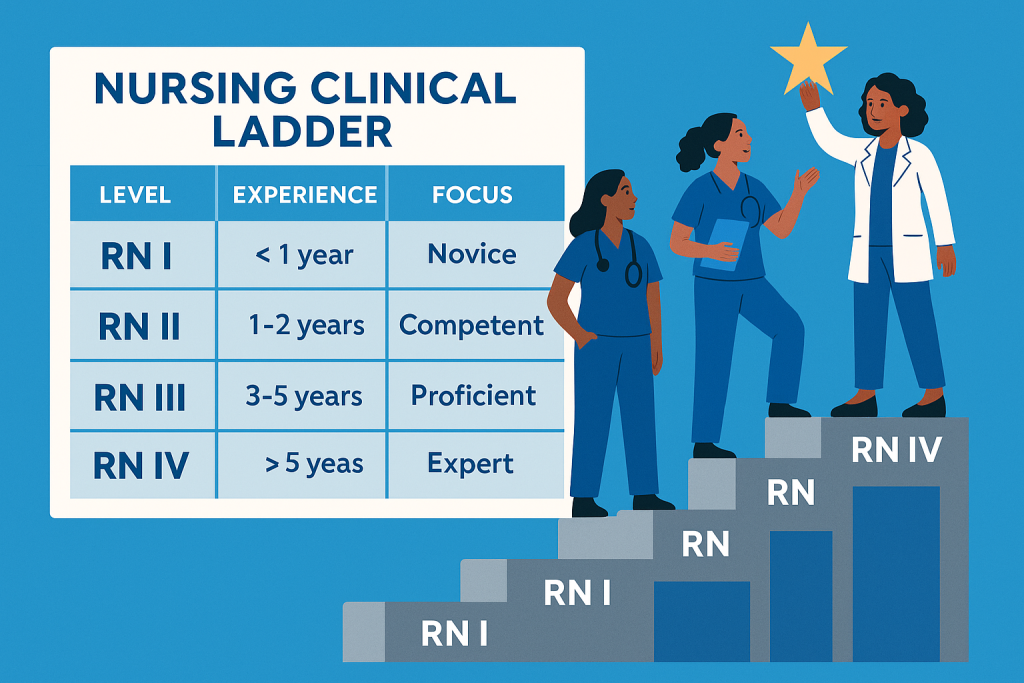
It outlines distinct levels of achievement — such as RN I, RN II, RN III, and RN IV — each marking higher skill, leadership, and contribution to patient care.
Unlike a traditional promotion that changes your title or department, the ladder helps you grow within your current role. You stay at the bedside, but your experience, leadership, and initiative are formally acknowledged — often through a new title, salary increase, or bonus.
Its main purpose:
- Keep experienced nurses challenged and engaged.
- Reward excellence in clinical practice, teaching, and mentorship.
- Provide a transparent path for professional advancement.
Hospitals benefit too. Strong ladder programs improve retention, morale, and the consistency of evidence-based care.
Benefits of a Nursing Clinical ladder
A good clinical advancement program in nursing is a partnership between nurses and their employers. Nurses gain recognition and development opportunities, while employers retain committed, high-performing staff.
For nurses:
- Recognition for skill, leadership, and initiative.
- Opportunities to grow as a preceptor, educator, or researcher.
- Higher pay, bonuses, and visibility within the team.
- Renewed sense of purpose and motivation.
For employers:
- Stronger retention and engagement.
- A system to identify emerging leaders.
- Better patient outcomes through ongoing development.
- Support for Magnet or Pathway to Excellence goals.
In short, the nursing clinical ladder builds a workplace where talent doesn’t just stay, it thrives.
Typical Structure and Levels
Most RN clinical ladder levels follow four main tiers:
| Level | Common Title | Experience | Key Focus |
| RN I | Novice | < 1 year | Learning standards and unit routines |
| RN II | Competent | 1–2 years | Safe, independent practice |
| RN III | Proficient | 3–5 years | Leadership, mentorship, QI projects |
| RN IV | Expert | 5 + years | Advanced leadership, research, education |
While naming varies — some hospitals use Clinician I–IV — the goal is consistent: to make professional growth visible and achievable. You’ll see how this structure translates in practice as we look at real nursing clinical ladder examples from hospitals that have turned these tiers into thriving career pathways.
Real-World Examples of Clinical Ladders
It’s one thing to read about clinical ladders in theory — it’s another to see them in action.
These nursing clinical ladder examples show how real hospitals design programs that reward growth, boost morale, and keep nurses engaged.
UAMS Health – Clinical Ladder Example
| Category | Details |
| Institution | UAMS Health (University of Arkansas for Medical Sciences) – Nurses Clinical Ladder Program UAMS Health |
| Program Purpose | Provides a structured framework for nurses’ career development, from novice to expert, aligned with Benner’s novice‑to‑expert model. UAMS Health |
| Levels/Tiers | RN NG – Novice/Beginner: 0–12 mos experience RN I – Advanced Beginner: 12–24 mos experience RN II – Competent: 24–36 mos experience RN III – Proficient: 3+ yrs experience (expected level for all RNs at UAMS) RN IV – Expert (optional): 4+ yrs experience, BSN req’d RN V – Expert (optional): Graduate degree req’d UAMS Health+1 |
| Progression Basis | Annual performance appraisals and professional portfolio evidence (reflects competencies and growth). UAMS Health |
| Role & Competency Expectations | Expectations increase with each level: safe practice (RN NG), independent coordination (RN I), clinical leadership and analysis (RN II/III), and expert practice with evidence‑based change or leadership (RN IV/V). UAMS Health |
| Education & Certification Requirements | BSN required for RN IV; graduate degree needed for RN V; national certification encouraged across levels (often tied to pay differentials). UAMS Health+1 |
| Incentives/Opportunities | Hourly pay differentials for certifications; leadership/clinical project roles; portfolio development to document achievements; optional advanced expert tracks. UAMS Health+1 |
| Participation | Automatic placement upon hire based on experience, skills, and competencies; voluntary progression beyond RN III. UAMS Health |
| Why It Works | Clear expectations tied to clinical growth; supports nurse autonomy, leadership, and long‑term professional development; aligns with Magnet principles of excellence. UAMS Health |
InterMed Clinical Transformation Ladder
| Category | Details |
| Institution | InterMed – Clinical Transformation Ladder Program intermed.com |
| Program Purpose | Recognizes and rewards clinical staff for advancing professional knowledge, promoting quality care, leading improvement efforts, and demonstrating leadership across clinical practice. intermed.com |
| Eligibility | Clinical staff working in participating departments; must be in good standing with satisfactory performance review; part‑time/minimum hours requirements apply. intermed.com |
| Primary Roles Eligible | Registered Nurses (RNs), Licensed Practical Nurses (LPNs), Medical Assistants (MAs), Athletic Trainers (ATCs) (table below focuses on RN pathway). intermed.com |
| RN Clinical Ladder Levels | Level 1 – Entry: Meets core job responsibilities. Level 2: Functions independently; begins leadership contributions. Level 3: Advanced clinical expertise; leads or contributes to quality improvement; ongoing professional development required. Level 4: Clinical resource and leader with specialty/advanced practice focus. intermed.com |
| Key Advancement Criteria | Combination of: years of experience, education (BSN/MSN), national certification, and completion of required ladder domains (Quality/Lean Improvement; Professional Development; Leadership/Teamwork activities). intermed.com |
| Portfolio / Documentation | Candidates submit application elements including: letter of intent, support letters, resume, personal narrative, and documented evidence of domain activities. intermed.com |
| Domains & Activities | Quality/Lean Improvement: e.g., Lean Six Sigma participation, measurable improvement projects.Professional Development: Certifications, formal coursework, educational hours.Leadership/Teamwork: Precepting, committee participation, team engagement, volunteer work, policy development. intermed.com |
| Incentives/Recognition | Advancement is tied to professional recognition and expanded roles; maintenance and level‑related differentials may apply per HR policy (not universally specified in the guide). intermed.com |
| Why It Works | Encourages nurses to deepen clinical expertise, contribute to quality and leadership initiatives, and document professional growth through a structured, competency‑based process — helping retention and career engagement. intermed.com |
Central Washington Hospital (Confluence Health) – Clinical Ladder Example
| Category | Details |
| Institution | Central Washington Hospital / Confluence Health Nursing Clinical Ladder Program WSNA |
| Program Purpose | Voluntary recognition program supporting professional nursing growth, quality practice, and shared governance. WSNA |
| Structure / Levels | Level 1 – Clinical NoviceLevel Level 2 – Clinical ColleagueLevel Level 3 – Clinical MentorLevel Level 4 – Clinical Leader Level 5 – Clinical Expert WSNA |
| Experience Requirements | Varies by level: Level 2 (≥1 yr experience), Level 3 (≥2 yrs), Level 4 (≥3 yrs), Level 5 (≥4 yrs) WSNA |
| Point‑Based Criteria | Advancement requires accumulating points from education, professional development, clinical leadership, quality improvement, research/EBP, and shared governance activities. WSNA |
| Incentives | Level 2: $300 bonus Level 3: $1,500 bonus Level 4: $3,000 bonus Level 5: $4,000 bonus WSNA |
| Typical Qualifications | Licensure, performance review rating meets/exceeds standards, education level (BSN/MSN), certifications, portfolio documentation and activity points. WSNA |
| Why It Works | Combines recognition + financial incentives with structured expectations and measurable criteria; encourages ongoing professional engagement, leadership, quality improvements, and evidence‑based practice. WSNA |
Providence St. Vincent Medical Center – Clinical Ladder Example
| Category | Details |
| Institution | Providence St. Vincent Medical Center (Portland, Oregon) Clinical Ladder Program YMAWS |
| Program Purpose | Recognize nursing excellence, professional growth, and contributions that go beyond basic role expectations, aligned with a Benner novice‑to‑expert continuum. YMAWS |
| Eligibility | Contract nurses with demonstrated competence — Competent/Proficient/Expert depending on level applied for; no corrective action in prior year. YMAWS |
| Ladder Levels | Level I: Independent practice Level II: Resource/mentor role Level III: Role model and informal leader Level IV: Advocate for clinical excellence in specialty practice YMAWS |
| Advancement Criteria | – Portfolio submission with exemplar narrative and documented activities- Increasing nursing education hours required at each level- Demonstrated clinical judgments, teaching, collaboration/teamwork aligned with performance standards YMAWS |
| Portfolio Focus | – Varies by level from clinical skills to leadership in evidence‑based practice projects- Documentation must be current (past 12 months)- Word count expectations increase by level (e.g., Level I: 500–1500 words; Level IV: 2000–3500+ words) YMAWS |
| Assessment Domains | – Caring Practice (patient/family advocacy and communication)- Clinical Knowledge & Decision Making- Collaboration & Teamwork with Healthy Work Environment standards YMAWS |
| Why It Works | Emphasizes individual demonstration of higher‑order nursing practice — not just tenure — through structured portfolios, teaching initiatives, clinical leadership examples, and contributions to unit goals. YMAWS |
Each model proves one thing: when growth is visible, nurses stay inspired to climb higher.
Incentives & Pay Implications
One of the biggest motivators behind a nursing clinical ladder program is that it rewards real effort — not just seniority. Recognition matters, but it feels even better when it shows up in your paycheck and career growth.
How Ladders Tie to Pay and Recognition
As you climb each level of your hospital’s clinical advancement program, you may gain:
- Pay increases (usually 2–5%).
- Annual bonuses or stipends.
- Public recognition through award events.
- Access to leadership training and conference funding.
For instance, at MU Health Care, nurses who advance from RN II to RN III can receive up to a 5% salary differential, a title upgrade, and funding for certifications or conferences.
Each system is different, but the message is the same — growth deserves reward. Hospitals use these incentives to thank nurses for developing their skills, mentoring others, and staying engaged.
The benefits go beyond money. Nurses on higher rungs often enjoy:
- More confidence and credibility.
- Priority for leadership roles or committees.
- Greater fulfillment and less burnout.
When your work is recognized and rewarded, it’s easier to stay motivated and committed to your profession.
Frequently Asked Questions (FAQs)
Before you start climbing your nursing clinical ladder, let’s clear up a few common questions nurses often ask.
Do I need a BSN to join a clinical ladder?
It depends on your hospital. Many programs let ADN-prepared nurses start at RN I or RN II, but they often require a BSN for RN III or RN IV levels.
If you’re still finishing your degree, don’t wait to start your clinical ladder portfolio. Most programs allow you to advance once your BSN is in progress — and that initiative shows leadership.
Is participation mandatory?
Usually not. Most hospitals make participation voluntary, but joining has clear benefits:
- Better pay and recognition.
- Stronger evaluations.
- More visibility for promotions and committees.
Think of it like this — you can keep walking, or you can start climbing. The ladder gives you visible steps for career growth.
How long does it take to move up to RN III or RN IV?
It varies, but most nurses progress within three to five years through steady engagement in leadership, education, and QI projects.
A general timeline:
- RN I → RN II: First year, after orientation.
- RN II → RN III: About 2–3 years of independent practice and mentoring.
- RN III → RN IV: Roughly 4–6 years with proven leadership or advanced specialty work.
Your pace depends on how actively you participate — committee work, CEUs, or precepting can speed it up.
What happens if I don’t participate?
Nothing punitive — but you’ll miss out on recognition and opportunities. Hospitals often prioritize ladder participants for bonuses, special projects, or leadership roles.
Even if you’re not applying right now, document your achievements. That portfolio can become gold later when new positions open.
Can I move backward if I don’t maintain my criteria?
Yes, and it’s more common than you’d think — but it’s not a punishment. Many programs require annual reviews to keep levels meaningful.
If you fall short on continuing education or projects, you might revert to a previous level until you catch up. The goal isn’t to penalize but to keep standards high and progress ongoing.
Does every hospital have a ladder?
Not all. Larger systems and Magnet-recognized hospitals are more likely to run structured clinical advancement programs, while smaller facilities may use informal recognition models.
If your hospital doesn’t have one yet, use these nursing clinical ladder examples to start the conversation. Many programs began because one nurse asked, “Why not us?”
Conclusion & Next Steps
At its core, the nursing clinical ladder is about recognizing growth — the daily moments that shape you into a stronger, wiser nurse. Every new grad you’ve mentored, every project that made care safer, every certification you’ve earned — these are milestones worth celebrating.
When done well, a clinical ladder program becomes a win for everyone:
- For nurses: it validates hard work, builds confidence, and opens doors to higher pay and leadership.
- For organizations: it boosts retention, morale, and quality of care.
If you’re ready to start climbing:
- Review your hospital’s ladder criteria — or ask your manager for them.
- Create a simple folder for certificates, exemplars, and feedback.
- Talk to a mentor who’s advanced through the program and learn from their path.
And if your workplace doesn’t have a ladder yet, don’t wait for someone else to suggest it. Use the nursing clinical ladder examples from this guide to build your case and spark change.
Professional growth isn’t about racing ahead — it’s about taking the next meaningful step. Keep climbing. Every rung you reach helps you, your patients, and your profession rise higher.

