You explained it clearly. Slowly. Maybe even twice.
The patient nodded, said “okay,” and you moved on.
Then they came back.
The wound wasn’t cleaned correctly. The inhaler was used wrong. The medication schedule was misunderstood. And suddenly, you’re reteaching something you were sure you covered.
Patient education doesn’t fail because nurses don’t care. It fails because knowing what to teach isn’t the same as knowing how to teach it in the middle of a busy shift.
That’s where this guide comes in.
Below, you’ll find real-world patient education nursing examples that show what to teach, exactly how to say it, and how to check that it actually stuck. These aren’t long lectures or ideal scenarios. They’re short, practical teaching moments you can use while hanging an IV, preparing a discharge, or managing multiple patients at once.
Expect simple scripts, 10 distinct scenarios, and complete teaching plans designed to be scanned, adapted, and used immediately.
What Patient Education in Nursing Really Means
Patient education isn’t about delivering information—it’s about making sure patients can actually use that information once you’re no longer there.
At the bedside, patient education means translating medical instructions into actions a patient can repeat, remember, and carry out safely at home. It’s the difference between hearing directions and truly understanding them.
When patients understand both the why and the how, everything changes. Medications are taken as prescribed. Warning signs are recognized earlier. Follow-up care feels manageable instead of overwhelming.
That’s where your role becomes critical.
As a nurse, you are the one who:
- Assesses what the patient already knows (and what they think they know)
- Identifies gaps in understanding
- Teaches in plain, human language—not textbook terms
- Checks for understanding, because nodding doesn’t always mean “I get it”
- Connects patients with resources and encourages independence
But here’s the challenge: patient education isn’t one-size-fits-all.
Effective teaching depends on the human in front of you. Every patient brings different needs, limitations, and barriers, including:
- Health literacy: Can they make sense of the instructions?
- Readiness: Are they in pain, anxious, or exhausted?
- Developmental stage: Teaching a child is not the same as teaching an older adult.
- Culture and language: Do background or language differences affect how information is received?
When you meet patients where they are, education sticks—and patients feel supported instead of overwhelmed.
10 Patient Education Nursing Examples
Understanding patient education is one thing. Putting it into practice is another.
The patient education nursing examples below show exactly how to teach in real clinical situations—clearly, quickly, and effectively.
1. Diabetes Mellitus
Scenario: Mr. K is newly diagnosed with Type 2 diabetes. He is staring at the glucometer and admits, “I’m scared I’ll do it wrong.”
Key Teaching Points:
- The “Why”: Explain that the glucose number is just a speedometer for his sugar levels—it tells him if he’s going too fast or too slow.
- The Steps: Keep it punchy: Wash hands → Insert strip → Poke side of finger → Apply blood → Read result.
- The Analogy: Teach insulin basics using the “Insulin is a Key” analogy. Insulin unlocks the door so sugar can leave the blood and enter the cells for energy.
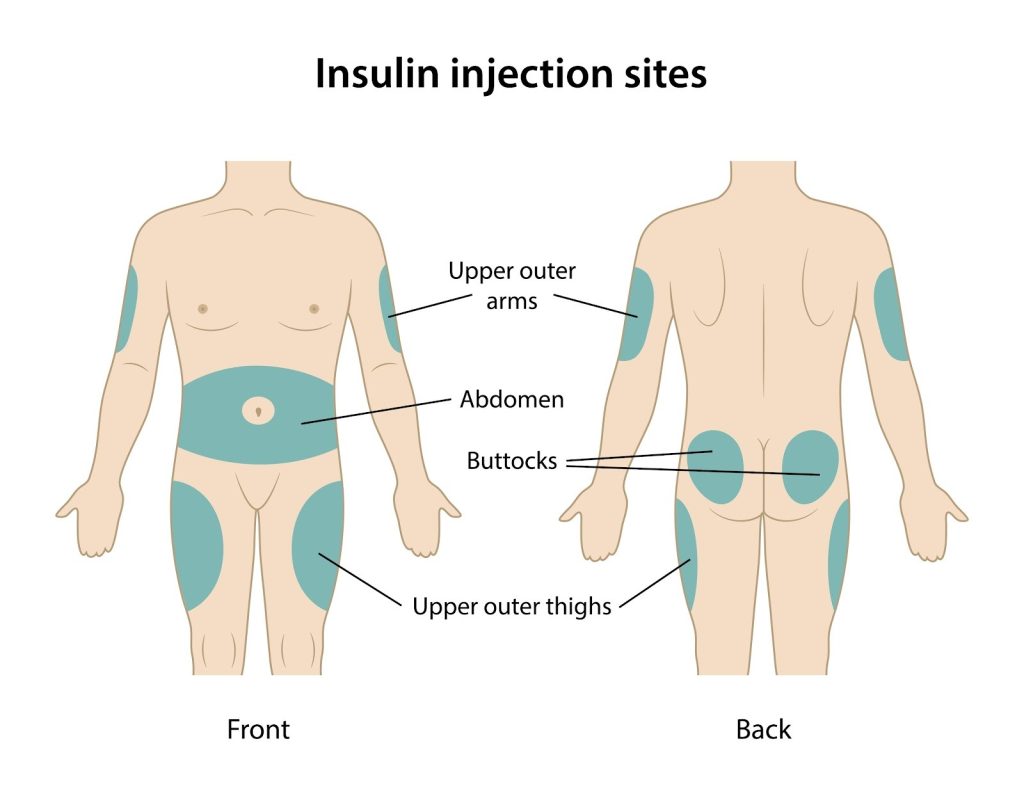
- Safety: Rotate injection sites to prevent lumps. A simple rule? “Don’t poke the exact same spot twice in a row.”
- Diet: “Half your plate should be vegetables.”
Return Demonstration: Mr. K successfully checks his blood sugar while talking through each step aloud and handles the lancet safely.
Documentation: “Taught glucose monitoring and insulin technique. Patient completed return demo and restated hypoglycemia signs.”
2. Hypertension (High Blood Pressure)
Scenario: Ms. L has uncontrolled blood pressure. She says she “tries to eat healthy” but is confused about what that actually looks like.
Key Teaching Points:
- The Sodium Sponge: Explain sodium simply: “Salt acts like a sponge. It holds extra water in your body, which pumps up the pressure in your pipes (blood vessels).”
- Label Reading: Show her specifically where to look for sodium on a nutrition label.
- BP Check: Demonstrate how to sit (feet flat, back supported) and where to place the cuff on the arm.
- Lifestyle: Encourage short daily walks and taking meds at the same time every day.
Return Demonstration: She places the cuff correctly on her arm and points out the high-sodium foods in her typical diet.
Documentation: “Reviewed sodium reduction and BP self-monitoring. Patient demonstrated correct cuff use.”
3. Heart Failure
Scenario: Mr. J is going home after fluid overload. He admits, “I never notice when my weight is changing.”
Key Teaching Points:
- The Scale is a Tool: Explain that sudden weight gain isn’t fat—it’s fluid backup.
- Routine: Weigh yourself every morning, after peeing, but before breakfast.
- The Red Flags: Call if you gain 2–3 lbs in a day or 5 lbs in a week, or if you feel short of breath.
- Fluids: Reinforce fluid limits (e.g., 1.5L/day) and salt restrictions.
Return Demonstration: He explains exactly how he will track his weight at home and lists the specific “warning zone” numbers that require a call to the doctor.
Documentation: “Provided HF teaching. Patient verbalized weight-monitoring plan and warning signs.”
4. COPD / Asthma
Scenario: A patient keeps puffing their inhaler rapidly, misting the air instead of their lungs.
Key Teaching Points:
- The Technique: Shake inhaler → Exhale all air out → Press canister → Slow, deep inhale → Hold for 5–10 seconds.
- The Analogy: “Think slow and steady—like you are sipping hot tea through a straw.”
- Aftercare: Rinse the mouth after steroid inhalers to prevent thrush.
- Triggers: Identify things like smoke, cold air, or dust that make breathing harder.
Return Demonstration: Patient repeats the inhaler steps, slowing down the inhale and holding their breath for the full count.
Documentation: “Reviewed inhaler technique. Patient demonstrated proper use without prompting.”
5. Post-Operative Care
Scenario: A patient is nervous about their incision. They tell you, “I don’t want it to get infected.”
Key Teaching Points:
- Hygiene: Keep the incision clean and dry.
- Activity: Respect the lifting limit—if the surgeon said “nothing heavier than a gallon of milk,” they mean it.
- Pain Management: Take pain meds before activity or physical therapy so moving is easier.
- Infection Signs: Look for the “Hot and Angry” signs: redness spreading, heat, pus, or fever.
Return Demonstration: Patient lists the signs of infection and describes their plan for keeping the incision dry during showers.
Documentation: “Taught incision care and infection signs. Patient verbalized understanding.”
6. Wound Care
Scenario: A patient needs to change a leg dressing daily but seems hesitant.
Key Teaching Points:
- Safety First: Hand hygiene before and after touching the wound.
- Clean Technique: Clean from the center (cleanest) outward to the edges (dirtiest).
- Handling: Open the new dressing carefully—don’t touch the side that goes on the wound.
- Comfort: Keep the leg elevated to stop throbbing and swelling.
Return Demonstration: Patient performs a full dressing change with minimal coaching.
Documentation: “Demonstrated wound care. Patient completed return demo with proper technique.”
7. Chronic Pain
Scenario: A patient feels hopeless, saying, “Nothing helps unless I take a pill.”
Key Teaching Points:
- Multimodal Approach: Meds are just one tool. Introduce heat/cold therapy, stretching, and deep breathing.
- Tracking: Encourage a “Pain Diary” to spot patterns—does weather or certain foods make it worse?
- Safety: Discuss avoiding alcohol while on pain meds.
- Schedule: Explain why staying ahead of the pain is better than chasing it.
Return Demonstration: Patient practices deep breathing exercises and chooses one non-drug method (like a heating pad) to try at home.
Documentation: “Taught multimodal pain strategies. Patient verbalized safe medication use and coping skills.”
8. Fall Risk
Scenario: An older adult is unsteady on their feet but insists on walking to the bathroom alone.
Key Teaching Points:
- Call Don’t Fall: Press the call light before getting up.
- Gear: Wear those non-slip socks.
- Environment: Keep the path to the bathroom clear of cords and clutter.
- Walker Tips: “Step into the box of the walker, do not hold it way out in front of you.”
Return Demonstration: Patient shows safe walker placement and verbally agrees to use the call light.
Documentation: “Reinforced fall precautions. Patient demonstrated safe ambulation with walker.”
9. Anticoagulants (Blood Thinners)
Scenario: A patient starting warfarin asks, “I bruise easily—should I be worried?”
Key Teaching Points:
- Gentle Care: Switch to a soft toothbrush and an electric razor to prevent bleeds.
- Meds: Avoid NSAIDs (like ibuprofen) unless the doctor says it’s okay.
- The Signs: Watch for bleeding gums, pink urine, black/tarry stools, or nosebleeds that won’t stop.
- Diet: You can eat greens (Vitamin K), but keep the amount consistent. Don’t binge on salad one week and skip it the next.
Return Demonstration: Patient names three bleeding precautions and knows exactly when to call the provider.
Documentation: “Taught anticoagulant precautions. Patient restated bleeding risks and safety steps.”
10. Antibiotics
Scenario: A teenager with a sinus infection says, “I’ll stop the antibiotics once I feel okay.”
Key Teaching Points:
- Finish the Course: Explain that if you stop early, the strongest bacteria survive and multiply.
- The Zombie Analogy: “If you stop halfway, the bacteria come back like zombies—harder to kill next time.”
- Reactions: Teach the difference between side effects (upset stomach) and allergic reactions (rash, trouble breathing).
- Gut Health: Suggest yogurt or probiotics to help the stomach.
Return Demonstration: Patient explains, “I need to finish all the pills even if I feel better.”
Documentation: “Reviewed antibiotic use and allergic signs. Patient used teach-back correctly.”
Documenting Patient Education
What to Include
We all know the saying: “If you didn’t chart it, you didn’t do it.” Teaching is only half the job; documenting it protects your license and ensures the next nurse doesn’t have to start from scratch.
A simple formula to keep your charting quick and bulletproof is: Assessment → Teaching → Response → Follow-Up.
When you open that chart, make sure you capture:
- The Topic: What skill or knowledge did you cover?
- The Method: Did you use a demo, a video, or a handout?
- The Evidence: How do you know they understood? (e.g., “Patient performed return demo”).
- The Barrier: Was there pain, confusion, or a language barrier?
Short, Realistic Documentation Examples
Here is how to use patient education nursing examples in your actual charting notes:
- Diabetes: “Reviewed glucometer use and insulin steps. Patient completed return demonstration safely and restated signs of low blood sugar. Provided written instructions for home.”
- Wound Care: “Taught clean technique for dressing changes. Patient performed full return demo with correct steps. Identified three infection signs. Will reinforce tomorrow.”
- Anticoagulant Safety: “Discussed bleeding precautions, dental care, and vitamin K consistency. Patient verbalized when to seek help. Provided printed bleeding precautions sheet.”
- Fall Prevention: “Reviewed fall-risk safety measures. Patient demonstrated correct walker use and agreed to use call light before getting up.”
Why It Matters: Good documentation stops duplicated teaching and highlights safety risks before they become readmissions.
Barriers to Patient Teaching and Quick Solutions
Even the best teaching falls flat if a patient isn’t ready to learn. Nurses run into the same walls every shift: pain, fatigue, anxiety, and the clock ticking down.
Here is how to spot the barriers and the “Quick Fixes” to get around them.
| The Barrier | The Quick Fix |
| Pain | Treat the pain first. Teaching is useless if they are hurting. Come back 30 minutes after medication. |
| Fatigue | Keep it short. Teach during “up” times (like after breakfast), not when they are exhausted. |
| Anxiety/Fear | Acknowledge it. A simple “Is now a good time?” gives them control. If they are overwhelmed, focus only on immediate safety. |
| Language | Use an interpreter immediately. Don’t rely on family members for complex medical info—it’s unsafe. |
| Time Crunch | Prioritize. If you have 2 minutes, teach the one thing that keeps them safe tonight. Break the rest into small chunks later. |
| Low Literacy | Ditch the text. Use visuals, photos, and hands-on practice. Show, don’t just tell. |
In Conclusion
Patient education is one of the most powerful tools in your kit. It isn’t always dramatic, and it doesn’t always happen in a classroom setting. It happens in the quiet moments—while you’re changing a dressing or handing over a prescription.
When you help a patient understand why they are taking a pill or how to care for their body, you aren’t just giving instructions. You are reducing their anxiety and giving them control back.
Use the patient education nursing examples in this guide as your starting point. Adapt the scripts, use the analogies, and don’t be afraid to keep it simple. At the end of the day, it’s not about using big words; it’s about making sure your patient walks out the door feeling ready for what comes next.
Frequently Asked Questions About Patient Education in Nursing
What are patient education nursing examples?
Patient education nursing examples are real-life teaching situations where nurses explain health information in a way patients can understand and apply. These examples often include medication instructions, disease management teaching, wound care education, and safety guidance, along with teach-back or return demonstrations to confirm understanding.
Why is patient education important in nursing practice?
Patient education is essential because it directly affects patient safety, treatment adherence, and recovery outcomes. When patients understand what to do and why it matters, they are more likely to follow care plans correctly and recognize warning signs early, reducing complications and avoidable readmissions.
What is the nurse’s role in patient education?
The nurse’s role in patient education includes assessing what the patient already knows, identifying gaps in understanding, teaching in plain language, and verifying comprehension using methods like teach-back. Nurses also adapt education based on the patient’s readiness, health literacy, and cultural background.
How do nurses evaluate whether patient education was effective?
Nurses evaluate patient education by observing return demonstrations, asking patients to explain instructions in their own words, and assessing whether patients can correctly describe warning signs or next steps. Teach-back is one of the most commonly tested and expected evaluation methods in nursing education.
What are common patient education topics in nursing assignments?
Common patient education topics include:
- Medication administration and side effects
- Chronic disease management (diabetes, hypertension, heart failure)
- Use of medical devices (inhalers, glucometers, walkers)
- Wound care and infection prevention
- Fall prevention and home safety
These topics frequently appear in nursing exams and written assignments.
What barriers affect patient education in nursing?
Common barriers include pain, fatigue, anxiety, low health literacy, language differences, and limited time during clinical shifts. Effective nurses recognize these barriers and adjust their teaching approach by shortening sessions, using visuals, involving interpreters, or prioritizing safety-critical information.
How should patient education be documented in nursing care?
Patient education documentation should include what was taught, how it was taught, how the patient responded, and any barriers identified. Many assignments expect documentation using a structure such as assessment, teaching provided, patient response, and follow-up plan.
What is an example of ineffective patient education?
An example of ineffective patient education is when a patient agrees verbally but cannot demonstrate or explain the instructions afterward—such as using an inhaler incorrectly or misunderstanding medication timing. In nursing scenarios, this signals the need for reinforcement and alternative teaching strategies.
How are patient education nursing examples used in exams and assignments?
In exams and assignments, patient education nursing examples are often used to test a student’s ability to identify appropriate teaching content, choose the correct teaching method, evaluate understanding, and document education accurately. Many questions focus on teach-back, safety priorities, and patient-centered communication.

